Antiracism in Healthcare |
|
Dennis H. Novack, MD. Associate Dean of Medical Education at Drexel University College of Medicine Camille Burnett, PhD, MPA, APHN-BC, BScN, RN, DSW, FAAN, CGNC Vice President | Health Equity | US Equity Portfolio, Institute for Healthcare Improvement 
|
|
© by Drexel University College of Medicine
|
Dennis H. Novack, MD
When you have completed this module and associated workshops, you will be able to:
-
explain how structural, cultural, and individual racism have shaped our common history and have led to vast societal disparities in education, policing, wealth and healthcare;
-
commit to being antiracist in your attitudes and behaviors;
-
contribute to creating an antiracist learning culture for healthcare trainees that honors diversity, equity and inclusion: where all trainees are respected, where faculty model respect and empathy for all patients, colleagues and staff, and where trainees feel empowered to contribute to a culture of mutual learning;
-
provide examples of how your increased self-awareness and reflection have helped you recognize your individual and cultural biases and how you use this awareness to seek to understand and empathize with your patients and clients of color, and to deliver equitable care to all;
-
have the moral courage to act as an ally and upstander for your minoritized colleagues and patients;
- use your understanding of structural, cultural and individual biases to advocate for positive changes in your institutions and communities that will lead to equitable care for all.
We hope this module will guide you in thinking about and executing ways
to engage holistically with your patients/clients as full, authentic beings.
By examining historical, social, economic and political forces that shape medicine
and human health, we offer ways in which to reconceptualize healthcare through
a social justice framework.
The first premise of this framework is that health practice must be truly patient-centered;
and that happens when the whole patient is seen. All patients' intersectional identities
shape their experiences and particularly inform their experiences with health and healthcare.
Two foundational principles of
do no harm
and
diversity drives excellence
have helped shape and inform the orientation of this module.
Too often in Western medicine, we separate the person from the disease, and when we do this,
we do harm. The intent of seeing disease, rather than the person, could be seen as promoting
equity in care. However, this perspective only reinforced existing structures of
bias and ultimately created greater healthcare disparities. The structures of dominance
within a society are mirrored in that society's healthcare system.
When a society is at its best, the disparities in healthcare may be minimized, but remain.
When a society is not at its best, the disparities in healthcare are exponentially worse.
The cost and damage are exponentially worse (National Center for Health Statistics, 2015).
Fortunately, all social systems are created and run by members of society and thus can
be changed and improved. As participants in the U.S. healthcare system, we are
both responsible for and capable of bettering this system. Establishing a social justice
framework for healthcare provides specific approaches to decreasing disparities and dismantling
structural inequities, such as racism. Racism is a public health issue and a root cause of
many inequities faced by minoritized populations, greatly affecting their health outcomes.
Therefore, learning about and understanding how to be anti-racist is a necessary competency
for all health providers.
Research shows that diverse groups are smarter, more innovative and reap greater financial rewards.
(Phillips, 2014). While the evidence is clear, the impact of inclusive and diverse practices
has far-reaching implications for the future of healthcare practice, our communities and for
the patients we serve. Leveraging diversity enhances the work we do, how we do it and with whom
we do it. Diversity facilitates new knowledge, ways of seeing and empowerment that are of
benefit to us all. We experience ourselves and each other in a more deeply connected way,
which allows all of us to practice to the fullest extent of our competencies.
For all these reasons, we welcome you to this module, so you can learn to cultivate diversity
in your teams, in your patient care and in your personal life. We believe that in doing so,
you will achieve excellence and more satisfying careers in healthcare!
Though it is now widely recognized that race is a social construct, biases and stereotyping based on outdated notions of biological differences persist in medical practice. Throughout American history prominent physicians have conducted (pseudo) scientific studies and contributed writings to "racial science" that have supported notions of inferiority of people of color. Physicians and physician organizations such as the AMA have been openly racist in the past. Times are changing, though, and today’s healthcare students and providers can lead the way in providing just and equitable care to all.
Would you consider yourself racist?
Perhaps the great majority of healthcare providers would deny that they are racist or let
biases influence their patient care. Yet there are great disparities in healthcare and health
outcomes between racial groups. Certainly, structural racism accounts for many of these disparities,
i.e., policies that have affected access to care, insurance coverage, biases in hiring and lending
that suppress earning potential of people of color and much more. Many studies suggest, though,
that racism is a fundamental cause of adverse health outcomes for racial/ethnic minorities and
racial/ethnic inequities in health. Williams provides an overview of the evidence linking the
primary domains of racism—structural racism, cultural racism and individual-level
discrimination – to mental and physical health outcomes (Williams et al., 2019). And many
studies suggest that our country’s long history of racism has influenced healthcare providers
to adopt unconscious racial biases that can affect patient care (Cooper et al., 2012;
FitzGerald & Hurst, 2017; Maina et al., 2018).
Racism is present in healthcare training.
Despite the modern understanding of race as a social
construct, basic science courses often present race in biologic terms (Tsai et al., 2016).
Racial biases that are common in the lay public are also common among medical trainees.
In one study, 50 percent of White medical students and residents held false beliefs about
biologic differences between Black and White people (Hoffman et al., 2016). There is a high
prevalence of workplace discrimination experienced by physicians of color, particularly Black
physicians and women of color, associated with adverse effects on career, work environment and
health (Filut et al., 2020). Discrimination by patients and colleagues based on skin color appears
to be common experiences of nurses as well (Wheeler et al., 2014). Students of color experience
higher levels of mistreatment by faculty than White students (Hill et al., 2020). Students who
are underrepresented in medicine are at greater risk of poor personal well-being, increased stress,
depression and anxiety (Hardeman et al., 2016). Burnout is common among resident physicians,
which can increase the expression of prejudices associated with racial disparities in healthcare
(Dyrbye et al., 2019).
How did it get this way?
While there has been spectacular progress in biomedicine, much
of the progress has come at a cost to Black and Brown people. Until the modern era, there
has been less attention to the science and art of attending to the personhood of patients and
even less to the healing potential of the relationship between patient and provider. Teaching
empathy, compassion and social justice in healthcare training is a relatively modern phenomenon.
Before the 1970s, biomedicine ruled with patients being objectified and basically serving as the
battlegrounds on which doctors and disease fought. Healthcare providers must be able to separate
themselves from the personhood and suffering of others to dissect a cadaver, to cause pain to heal
and to make objective decisions. Yet throughout the history of medicine in the U.S., this capacity
for objectification allowed physicians to be affected by prevalent stereotypes of Black and
Indigenous people and others of color, to see them as "others," to withhold empathy and to
influence their science and their patient care.
By 1619, when the first enslaved people arrived in Jamestown, Virginia, persistent negative
characterizations of Black people and people of color, in general, have justified enslavement,
violence, unconsented experimentation, forced sterilization, discrimination in housing, employment,
healthcare, incarceration and much more.
There is controversy about the origins of the idea of race. But Ibram Kendi argues persuasively
that the social construction of race began in the early 15th century with the expansion of the
African slave trade by Prince Henry the Navigator of Portugal. His biographer, Gomes Eanes de
Zurara, created blackness by lumping together the various shades of brown and the ethnic groups
that were being enslaved by his patron, Prince Henry. He described these enslaved peoples as
bestial and slothful, and believed that enslaving them and bringing them Christianity would
elevate them. The idea that blackness defined a group of people who were inferior and deserved
to be enslaved spread widely and justified the lucrative slave trade (Kendi, 2016). Beliefs in
the inferiority and other negative stereotypes of Blacks were enshrined in a steady series of
laws and social policies that have persisted until the present.
Physicians played an important role in supporting notions of the inferiority of Blacks, and
others of color, including the notion that Indigenous people were savages.
Physicians were
clearly influenced by widespread racial stereotypes and the acceptability of slavery.
(For example, 12 of the first 18 presidents were slaveholders.) Though there were many healthcare
providers who spoke out against slavery, slavery persisted for almost 250 years until its ending
during the Civil War. And the entrenched biases of many in the North and South that justified
slavery for so long persisted in Jim Crow laws (state and local laws that legalized enforced
segregation and marginalization of Black people), government policies and the suppression of
the Black vote until the Civil Rights Act in 1965. This law federally guaranteed Black
enfranchisement, but that right has been whittled away ever since. Lynching throughout the South,
as a means of terrorizing and keeping Black communities from advocating for their rights as
citizens, persisted until the 1950s.
Only in 2022 has a federal law been passed that labels lynching as a hate crime.
And modern-day lynching (public killing of an individual who has not
received due process), still occurs. Physicians are members of communities and are influenced
by the dominant culture. They have not, until recently, been at the forefront of protest and
change of structural racism.
In the 19th century, prominent physicians such as Samuel Morton, Louis Agassiz and Samuel
Cartwright "proved" through their (pseudo) scientific studies that Blacks were animalistic,
unintelligent, strong and designed for subtropical servitude. Morton, a prominent Philadelphia
physician, through his studies of skulls in the early 19th century, claimed that each of five
races had separate origins and that a descending order of intelligence could be discerned by
different skull sizes that placed Whites at the pinnacle and Blacks at the lowest. His work was
critical in "scientific racism," furthered by Agassiz, a professor at Harvard, who promoted
creationism, argued against Darwin’s ideas and supported human polygenism, that Whites and
people of color descended from different ancestors, fundamental to racist theories of the
inferiority of Black people and others of color. Cartwright, a prominent physician and medical
writer in antebellum New Orleans is remembered for his theories of "drapetomania," the disease
that causes enslaved people to run away; "rascality," the disease that made enslaved people
commit petty offenses; and "dysaesthesia ethiopica," which made enslaved people indifferent
and insensible to punishment. These and other writings that taught the inferiority of Black
people were enshrined in medical textbooks that guided young healthcare trainees
(Byrd & Clayton, 2001).
J. Marion Sims, President of the American Medical Association (AMA) in 1876, and
considered the father of modern gynecology, honed his innovative surgery by operating on
enslaved Black women without their consent and without anesthesia. Scientific racism made
possible the rise of eugenics, the notion that selected breeding could improve the human race,
which led to forced sterilization to maintain the purity and dominance of Whites by limiting
reproduction of people with undesirable traits, often people of color. Nazi Germany adopted
eugenics with the extermination of Jews and many others. Eugenics was supported by many U.S.
physicians. During the time of government sanctioned and supported forced sterilization from 1907
to 1981, up to 150,000 people were sterilized by physicians. The Tuskegee study, in which Black
sharecroppers were recruited in 1932 for a study of the natural history of syphilis and were never
treated despite the wide availability of penicillin by 1947, was shut down in 1972, but did
irreparable damage to Black people’s trust in the medical profession. The AMA has a long history
of racist practices that kept Black physicians out of medicine’s mainstream, for example, by
excluding them from membership in the AMA. This created barriers to specialty training and
professional development for Black physicians, directly harming minoritized communities who
suffered from a dearth of access to qualified physicians. For example, in 1931, there were 25,000
subspecialty trained physicians in the U.S., and only two of them were Black. This is a history
that the AMA now acknowledges and is working to build an antiracist future (Association, 2021).
Much of America's foundational wealth was built on the labor of enslaved people and the genocide and appropriation
of the lands of Indigenous people. These actions were based on declaring that these people were "savages" and in other
ways inferior to White settlers and pioneers who were creating a new country. We must acknowledge that U.S. physicians
contributed to justifying racial attitudes and practices.
In this modern era of racial reckoning, we recognize that we are moral agents in healthcare. We not only have responsibilities to put our
patients first and to treat all individuals as equals, but to work for social justice. We have a responsibility to become aware of and change
our biases and behaviors to reflect the highest ideals of our professions. We have a responsibility to contribute to changing our institutions
and laws to realize the potential and benefits of diversity, equity and inclusion. Healthcare education has recently focused on trauma informed
care. So many of our patients have experienced adverse childhood experiences and other traumas that profoundly affect their health (Bellis et al., 2019).
If we can elicit and understand the biologic and psychologic effects of that trauma, we can fashion effective therapeutic approaches to care. Similarly,
our communities of color have undergone collective and individual traumas from structural and interpersonal racism. Recognizing and appreciating this
trauma allows us to be responsible participants in the healing of our individual patients and of the society in which we all live.
Prince Akpokiro, BSc
Dennis H. Novack, MD
Structural, cultural and individual racism enacts a severe toll on the health of Black, Indigenous and people of color (BIPOC) communities. This toll includes increased morbidity and mortality when compared to White communities due to many factors, including wide disparities in wealth, the ability to afford and access care, and inadequate healthcare delivery. We discuss the many causes of these disparities from government and private policies and the adverse psychophysiological effects of the stress of racism.
The COVID-19 pandemic highlighted racial health disparities. Black, Indigenous and Latinx Americans are more than twice as likely to be hospitalized and die from COVID than White Americans (Prevention, 2022). In a systematic review and meta-analysis of 293 studies, Paradies and colleagues (2015) determined that racism was associated with poorer general health, physical health and mental health. For many years, life expectancy for the Black population has been lower than for the White population, but by the height of the pandemic, the difference had increased to six years (Arias et al., 2021).
The authors go on to identify the many pathways that lead to poor health in minoritized communities: Wide earning and wealth gaps limit abilities to afford quality medical and dental care. In 2016, for every dollar of income that White households received, Hispanics earned 73 cents and Black people earned 61 cents. And racial differences in wealth are stunningly larger. For every dollar of wealth that White households have, Hispanics have seven pennies, and Black people have six pennies. Racial residential segregation, brought about by government and private policies such as redlining, mortgage discrimination, restrictive covenants and discriminatory zoning, concentrates poverty, limits job opportunities, delivers low quality education, lowers access to medical care, reduces access to healthy food choices and more. Many studies of unconscious bias show that BIPOC patients receive fewer procedures and poorer quality medical care than Whites (Williams, Lawrence, & Davis, 2019). Yearby and colleagues (2022) provide a detailed historical context and an account of modern structural racism in healthcare policy, highlighting its role in healthcare coverage, financing and quality.
There are many psychophysiological pathways that contribute to negative health outcomes of Black, Brown, Indigenous and other historically marginalized people. The lived experiences of BIPOC people who live and work in predominately White environments can be stressful. There is chronic stress related to frequent experiences of discrimination, microaggressions, microinvalidations and simply feelings of needing to constantly prove oneself as worthy in White dominant work and educational environments. This stress is associated with preclinical indicators of disease, including inflammation, shorter telomere length (indicating increased cellular aging), coronary artery calcification, dysregulation in cortisol and greater oxidative stress (Lewis et al., 2015). Self-reported discrimination has been linked to adverse cardiovascular outcomes, body mass index (BMI) and incidence of obesity, hypertension, engagement in high-risk behaviors, alcohol use and misuse, poor sleep, depression and maladaptive health behaviors, such as delaying care and reduced adherence to medical regimens (Thames et al., 2019; Williams, Lawrence, Davis, et al., 2019).
Systemic racism frequently results in persons of color and members of other oppressed ethnic groups not receiving the mental healthcare they require (Paradies et al., 2015). A survey of Black people who had not obtained formal care for a mental health issue found that respondents cited mistrust in mental health support systems because of racist experiences, stigmatization and that previous clinicians had downplayed their mental health concerns (Alang, 2019).
Using peer and community support, developing a strong sense of racial identity and talking about racist experiences can all be useful strategies of coping with racism's stress. Similarly, low socioeconomic status has negative health consequences that affect physical health and mental health (Stringhini et al., 2017). With the wealth gap and economic racial disparities among BIPOC populations, the cumulative impact of socioeconomic status further exacerbates these issues, with BIPOC people more likely to have mental health issues that last longer.
The stigmatization of mental health concerns can increase the impact of racism on Black and other oppressed communities' access to healthcare. Shame and stigma concerning poor mental health are ubiquitous in many communities, which often prevents those affected from seeking psychological help. The consequences of stigma are worse for racial and/or ethnic minorities, since they combine with other social adversities such as poverty and discrimination within policies and institutions (Eylem et al., 2020). All providers must be aware and practice with the knowledge of the intersecting factors that affect the health of their patients and those that plague communities of color that are rooted in racism and racist structures.
What is it about our psychology and our society that encourages the thriving of
racism, as well as all biases? So many biases are prevalent: homo- and transphobia,
anti-Muslim, anti-Asian, anti-immigrant sentiments, all "isms": sexism, ageism,
ableism and more. There are related questions: how did the people who founded the
United States justify, normalize and promote the enslavement of human beings?
How did they rationalize taking the lands of Indigenous people and participating
in their genocide? Since our country's founding there has been systematic
oppression and the creation of vast inequities between White people and people
of color. Are there particular processes common to the way humans think, feel
and organize their societies that allow and even encourage racism?
A biopsychosocial approach is the most effective way to understand and treat
patients' illnesses. Similarly, this approach can shed light on the questions
above. Racism is multidetermined and has complex origins, but we can summarize
a few key features of its origins in biology, psychology and the way we construct
our societies.
Though our reptilian, mammalian and then primate ancestors had been evolving for
about 320 million years, Homo sapiens emerged in Kenya and Ethiopia only 170,000
years ago. Their skins were certainly black, and all humans who are alive today
are descended from those people. We all have black ancestors. Some of our ancestors
migrated north, and over many years their skins became lighter to better
manufacture vitamin D. Fortuitous mutations in the genes that controlled facial
and tongue muscles emerged and facilitated the development of language.
Other mutations that promoted increased brain growth emerged about 40,000
and then again about 6,000 years ago. Transmission of knowledge, culture,
wisdom, the development of social structures and civilizations proceeded from
these advances. But certain survival reflexes and instincts that evolved prior
and subsequent to our emergence as Homo sapiens are still with us (Vaillant, 2008).
For all the years that we were hunter gatherers, our ancestors developed emotional
capacities that define us today. To survive in family groups and tribes, our
ancestors developed positive emotions of empathy, compassion, altruism,
love, hope, joy and faith. These emotions were critical to the success and
cohesion of family units and tribes, as well as the advancement of civilizations.
In harsh times of scarcity, though, fear gave rise to negative emotional states.
Selfishness, greed and dominance of others, competitiveness, fear of predators and
others who could harm us or encroach on resources, anger, the capacity to "otherize"
those who threatened us, and the use of violence were also survival strategies.
Seeing enemies as "others" allows us to close off empathy for their suffering.
Human history has been marked by a continual series of wars fueled by these
negative emotional states. Fear and other negative emotions are foundational in
the development of racism and other "isms." And protecting the integrity of one’s
tribe persists today.
A full discussion of the human psychology that might support racism is beyond the
scope of this section. There are some dynamics, though, that warrant special
attention.
Human children develop into adults within long periods of dependency. On the way
to achieving basic needs for autonomy, competence, and relatedness (Ryan & Deci,
2000), we go through developmental stages (Erikson, 1993; Kegan, 1982), each of which
promote or undermine our sense of trust and safety in the world, and our emerging
sense of competence, independence and self-esteem. Poverty, food and job insecurity,
and social and emotional stressors can disrupt parental effectiveness and optimal
development and promote the use of psychological defenses that support prejudice.
Also, in childhood, the need for love, safety and protection from helplessness and
vulnerability results in needs for affection, admiration for strong parental figures,
and a need to gain power through words and fantasy. The need to be powerful, which
we gain in relation to others, is a core dynamic in development and a core dynamic
in hierarchical societies, such as our own. Attraction to strong authority figures
is especially keen in times of societal instability, partially explaining the rise
of authoritarian leaders, some of whom play off our fears of "the others" who commit
crimes, take our jobs, or challenge our moral and religious views of right and wrong.
Innate needs for autonomy, competence and relatedness can best be realized within
stable societies. Many who benefit from the current structure have an investment
in the stability of their societies, whether or not they are just.
To deal with anxiety and fear, humans have developed a hierarchy of psychological
defenses, some of the most immature of which are projection and denial. (Mature
defenses include sublimation, humor, altruism, anticipation, suppression and
self-assertion (APA, 1994; Vaillant, 1977). Projection and denial protect our firmly
held beliefs from being altered by facts and blame others for our troubles. Denial
helps us, for example, ignore the reality of the findings of the human genome project
that there are no biologic differences between races. Race is a social construct.
We are one race – the human race. However, centuries of pseudoscience classifying
people by race, which justified the enslavement and oppression of people of color,
persist in our sensibilities today. Collective denial and projection can assure us
that our beliefs and prejudices are "true." Other psychological defenses include
isolation of affect, devaluing others and intellectualization, all of which can
contribute to racist thinking and behaviors.
Kegan's (1982) work on adult moral development is relevant. He posits five stages
of moral development and asserts that about 65 percent of the general population
never make it past Stage 3, in which our moral reasoning relates to perceived
cultural norms. If we are in Kegan’s Stage 3, we lack an independent sense of self,
because so much of what we think, believe and feel is dependent on how we think
others experience us. It is easy to see that if we grow up in a culture that benefits
from structural racism, we accept it because it is a cultural norm. We can be
mostly unbothered by the exploitation and oppression that makes our lives possible.
If we are middle class Whites, we seek to live in White dominated communities that
offer the best schools for our children. The fact that Black and other minoritized
children receive under-resourced and inferior education is regrettable but does not
move most of us to action. We benefit from cheap clothing made by forced labor of
Uighur people in China or from the palm oil in cookies made from palm kernels
picked by child laborers in Indonesia. If we are comfortable in our lives, other
concerns – our relationships and social lives, our children’s educational
achievements and sports activities, etc. – fill our worlds.
Another human capacity is relevant in support of racist ideas – our tendency to
stereotype. With so many facts and sensations coming at us all at once, our brains
cope by making snap judgments and by stereotyping. We are constantly judging and
assessing others so that they fit into our preconceived notions and world views.
Daniel Kahneman (2011) explains how we so often make cognitive errors in judgement,
and how we can be blind to the obvious and also blind to our blindness.
There is no reality except the reality that we construct with others and agree on.
We all have points of view that are limited by the scope of our vision, our family
and cultural values, our shared history, and what we learn in school and
in the media. Many of us learned that Columbus was a hero but didn’t learn that
he was an enslaver. Some of the men who died valiantly at the Alamo, Davy Crockett
and Jim Bowie among them, were also enslavers and were fighting so that Texans could
be free to enslave Black people. They were engaging Mexico’s President General
Santa Anna’s forces who were fighting for their land and who opposed slavery.
It is often said that history is written by the victors. Our heroic version of
our American history tends to neglect that our founders who crafted the legal
bases of our country were also protecting the wealth of rich landowning White men.
"All men are created equal" did not include women, Black people or Native Americans.
Hundreds of laws, court decisions, private actions and economic and political forces
reinforced the creation of structural racism over the last 400 years of our history
in North America.
It is not human nature to be racist. We have to be taught. However, we live
in a socially constructed reality that is supported by the dynamics of human
psychology, cognition and development. They are components of our shared human
nature that we can rise above. We create our lives within a society that supports
vast disparities in wealth and opportunities. Even among those who have become
aware and troubled about inequities, many do little to change the current order
or to speak up when they observe insensitive racial slights of others. As
healthcare providers, though, we can work to understand human nature better
than others. We can strive to advance our own moral development. And we can
use our knowledge and skills to advocate for just and equitable healthcare
for all.
R. Ellen Pearlman, MD, FACH
Critical Race Theory (CRT) was developed in the late 1980s by a group of legal
scholars. This group included Derrick Bell, Neil Gotanda and Kimberlé Crenshaw.
The core idea is that race is a social construct and that racism is not merely the
product of individual bias or prejudice but has become structural. Over hundreds
of years government policies and legal decisions reflected cultural attitudes about
minoritized groups to disadvantage them in housing, employment, education,
healthcare, the justice system, etc. There are other tenets of Critical Race
Theory, such as interest convergence, which stipulates that Black people achieve
civil rights victories only when White and Black interests converge.
Furthermore, racism in the United States is normal, not aberrational: it is the
ordinary experience of most people of color. Other tenets include "intersectionality"
recognizing that one’s racial identity is only one of many ways people may identify
themselves – and that multiple marginalized identities can be especially hurtful and
confusing to identity formation; that marginalized people are in a unique position
to tell stories about their lived experiences; and that people of color are
characterized at various times with different racial stereotypes, based on the
needs of the dominant White culture.
While a review of the history of race in this country would substantiate the
truth of these observations, many conservative politicians have demonized the
teaching of critical race theory. Yet this teaching is essential for healthcare
students, who are learning their professions in an unequal and unjust healthcare
settings, and who need to advocate for change. Tsai, Wesp and their colleagues
describe how CRT education can transform medical and nursing education (Tsai et
al., 2021; Wesp et al., 2018).
Let us further consider how these concepts apply to health systems. First,
U.S. health systems were developed from the ground up within racist frameworks.
The very fabric of how we deliver care and how we educate physicians is embedded
in structural racism. It is no wonder, then, that there are significant health
disparities in all aspects of healthcare.
The following video encapsulates the idea that race is a social construct:
• The Myth of Race Debunked in 3 minutes https://www.youtube.com/watch?v=VnfKgffCZ7U
Delgado, R., & Stefancic, J. (2017). Critical race theory: An introduction (Vol. 20). NYU press.
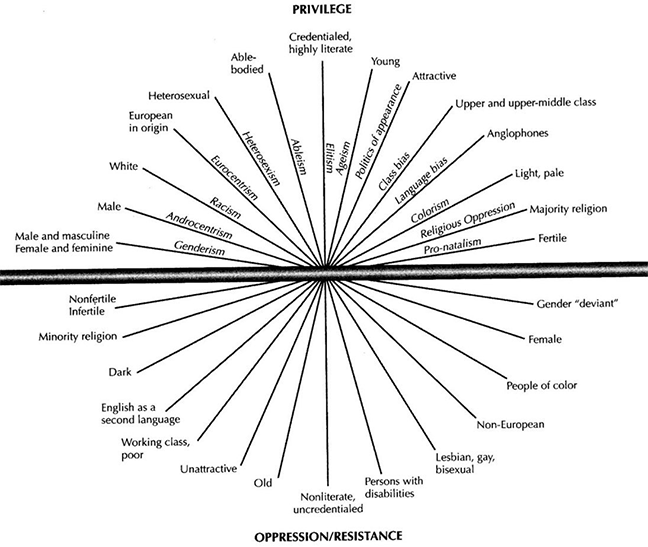
This concept was coined by legal scholar Kimberlé Crenshaw to explore the ways in which people with multiple marginalized identities experienced discrimination. The concept of intersectionality describes the ways in which systems of inequality based on gender, race, ethnicity, sexual orientation, gender identity, disability, class and other forms of discrimination "intersect" to create unique dynamics and effects. It is important to note here that intersectionality is not the "layering on" of identities; nor is it about any/all aspects of identity. Intersectionality focuses on identities that are marginalized and argues that the point of intersection between these marginalized identities results in an erasure of the individual that ultimately results in the person’s inability to find resolution to their experiences with discrimination. Bowleg (2012) points out that individual-level experiences of people at multiple marginalized intersections typically reflect social-structural systems of power, privilege and inequality.
Kimberlé Crenshaw's "Demarginalizing the Intersection of Race and Sex:
A Black Feminist Critique of Antidiscrimination Doctrine, Feminist Theory
and Antiracist Politics"
The Combahee River Collective Statement (1977)
This section addresses words we hear in popular media as "political terms" in
the culture wars. However, these words are actually rigorous theoretical frames
that directly address issues of culture, identity, privilege and power.
Colonialism is the process by which a government/nation occupies another nation
and claims that nation, its land, its people, its resources and its existence
for the benefit of the colonizing nation. Most often, these moves were justified
by referring to "the White man’s burden." This phrase referred to the responsibility
of "those made in the image of God" to bring civilization and salvation to savage and
uncultured corners of the earth. This allowed colonizers to treat the people of
colonized lands as "animalistic," "savage," uncivilized, uneducated, etc. While
colonialism has existed since ancient times, modern western colonialism began in
the mid-15th century when Prince Henry the Navigator of Portugal set up African
trading posts and initiated the African slave trade.
The impacts of colonization are immense and pervasive. Various effects, both
immediate and protracted, include the spread of virulent diseases, unequal
social relations, detribalization, exploitation, enslavement, medical advances,
the creation of new institutions, abolitionism, improved infrastructure and
technological progress. Colonial practices also spur the spread of colonist
languages, literature and cultural institutions, while endangering or
obliterating those of native peoples (Wikipedia).
While presumed that the era of colonialism has ended, colonialism is still
prevalent in current global politics and its impacts continue to reverberate
throughout the world. Colonialism goes beyond "the takeover" of a country. It
includes infiltrating the colonized country with the language, culture and values
of the colonizing nation. For example, the British imported their train system to
India. This was not simply the development of railroad systems for India. It also
carried with it the values of "time and efficiency," marking them as important
characteristics for a "successful" society. We see this in contemporary presumptions
such as "progress" and "life-saving techniques." Colonialism also includes the
taking of resources from the colonized peoples, which includes not only material
objects (such as gold, diamonds or copper) but also cultural knowledge and practices
and claiming them as "discoveries," negating the science and knowledge of ancient
cultures.
Colonialism set the groundwork for western science to be seen as the
"first" true science. It allowed for scientific discovery to be intertwined
with the "salvation" of uncivilized peoples. This then allowed western science
to describe non-western bodies and practices as inferior, as well as demonic,
deviant, diseased, and pathological. These attitudes infiltrated the development
of health systems and the care of marginalized people for centuries and persist
today.
• Albert Memmi's "The Colonizer and the Colonized"
• Franz Fanon's "Wretched of the Earth" and "Black Skin, White Masks"
Racism is overwhelmingly thought to be "bad acts and beliefs by bad people."
This frames it as an interpersonal, immoral, individual act. As the previous
sections of this module explain, racism, like race, is a socially constructed
phenomena and functions at society’s structural level. Individual, institutional
and social acts of racism manifest through sustained structures that create and
reinforce racism.
Structural racism in the U.S. can be defined as the normalization and
legitimization of an array of dynamics – historical, cultural, institutional
and interpersonal – that routinely advantage Whites while producing cumulative
and chronic adverse outcomes for people of color. It is a system of hierarchy and
inequity, primarily characterized by White supremacy.
Structural racism encompasses the entire system of White supremacy, diffused and
infused in all aspects of society, including our history, culture, politics,
economics and our entire social fabric. Structural racism is the most profound
and pervasive form of racism – all other forms of racism (e.g., institutional,
interpersonal, internalized, etc.) emerge from structural racism. Structural
racism has shaped the delivery of care and the science of medicine. For example,
many clinical algorithms used today are based on faulty or pseudoscientific
observations of racial differences. Nyas and colleagues (2020) argue that we
need to reconsider use of race corrections to ensure that our clinical practices
do not perpetuate the very inequities we aim to repair.
Gloria Yamato's essay "Something about it is hard to name", In Margaret L. Anderson and Patricia Hill Collins. eds. 2004. Race, Class, and Gender. 5th Ed. NY: Thomson/Wadsworth Pub. Pp. 99-103. (https://likeawhisper.files.wordpress.com/2010/03/somethingaboutthesubject.pdf)
Foundational concepts, principles, and duties guiding contemporary clinical ethics provide a clear mandate for antiracist action in the care of patients and communities. Key points for understanding include social contract, human rights, guiding ethical principles, essentials of caring, and virtue as personal commitment.
As members of healthcare professions, we are entrusted with
the lives and wellbeing of our patients. Each profession
enters into a binding contract with society. Society entrusts
clinicians with powers and privileges to care for patients.
As examples, society allows each profession sets its own
standards and training. Clinicians are permitted access to
patients’ bodies and personal information. We make treatment
decisions that have consequences for patients’ lives. We are
permitted unsupervised interaction with people during their
most vulnerable times. As a student or practitioner, you enjoy
these permissions and freedoms only because you are a member
of your healthcare profession.
In exchange, all members of every healthcare profession are
bound to a responsibility to serve the best interests of
patients and society. Clinicians are guided in this by ethical
principles and ethical commitments that have changed
dramatically over time and continue to evolve. The
emergence of autonomy and social justice as guiding ethical
principles are two key examples that mark a sea-change in
ethical thinking and action of antiracism in medicine and
healthcare.
Historically and until around the 1950s-1960s, guiding
principles in medical ethics were beneficence (doing the most
good for a patient) and non-maleficence (avoiding harm to that
patient). Physicians made treatment decisions based on their
professional understanding of what was good or bad for the
patient, often in disregard of patients’ values or choices.
In the US, the period around the 1960s was one of social
change driven by movements related to civil rights, feminism
and gender equality, rights of the incarcerated, rights of
human research subjects, and consumer rights. Historically
oppressed or disempowered groups demanded recognition as fully
equal members of society and self-determination—control over
one's own life and life decisions.
At the same time, rapidly emerging technologies such as
ventilators, organ transplantation, and radical surgeries
raised critical quality of life concerns: just because a
treatment could be done, does not mean it should be, especially
because the patient may not want to live with the consequences.
In both of these contexts, social and individual, autonomy
emerged as a central guiding principle of modern bioethics.
Autonomy means having control over one’s own body, mind, and
life decisions, free from oppression and coercion. It is a
human right.
As modern bioethics emerged during the 1960s and 1970s, the principle of social justice featured as another fundamental, guiding principle. The interpretation and application of this principle has continued to develop and has gained increasing prominence and significance. Applications of the social justice principle have always included the equitable distribution of limited healthcare resources (distributive justice). Social justice also always informed the negotiation between individual autonomy and health of the public: individual autonomy must be curtailed at times in the service of public health (e.g., quarantine, mandated vaccinations, mandatory reporting of certain diseases and conditions). Belatedly, mainstream clinical ethics has now intensified and broadened its understanding of social justice to also address structures of racism and other social oppression and practitioner bias as they relate to patient care and outcomes and the health of communities.
Quality clinical care and ethical care are inseparable.
It happens too often that an indicated treatment is provided,
but in a way that undermines autonomy, injures the patient
emotionally, and/or turns the patient away from seeking
necessary care in the future. This is unfortunately an
experience of BIPOC and other members of our community who
have suffered discrimination, bias, or stigmatization.
On a more macro level, a patient may be presenting with a
medical need that was caused or exacerbated by structural
barriers to the determinants of health and survival (healthcare,
food, income, education, safe housing, social integration).
A child of color may have uncontrolled asthma because of
unhealthy housing conditions resulting from generational
disenfranchisement and redlining that placed affordable,
healthy housing out of reach.
We must always see this inextricable joining of clinical and
ethical care. Clinical questions are: what is the correct
diagnosis and how do I administer the correct treatment?
Simultaneous ethical questions are: How do my words and
actions as a clinician respect patient autonomy, demonstrate
my trustworthiness, and reflect the appropriate management of
professional power to achieve the most good and avoid harm?
Clinicians view patient care through multiple ethical frames
that ultimately justify antiracist objectives. These are:
PRINCIPLES. As already introduced in this discussion,
contemporary clinical ethics employs guiding principles.
These include respect for persons, autonomy, beneficence
and non-maleficence, and social justice.
SOCIAL CONTRACT. Every patient interaction must fulfill
the promise of this contract, use professional power
and privilege only in the service of our patient.
This is a contract of trust and trustworthiness, and
all actions are to directly or indirectly promote trust.
Trust is the foundation of any patient encounter and we
do not take it for granted. We have come to increasingly
realize the complex roots of patient distrust of the
US medical system that include historic mistreatment
and abuse of black, indigenous, and other people of color.
VIRTUE. Clinicians must develop their own capacity to be guided
by ethical principles and uphold the social contract even
under challenging and difficulty circumstances. Throughout
our professional lives we deepen our capacities for
compassion, excellence, moral courage, and other moral
qualities in the service of patient care. Today we
realize this must include overcoming race and other
bias in ourselves, intervening to the extent we are
able when witnessing racism or discrimination in the
healthcare setting, and working to overcome structural
racism and other barriers to health equity.
Medical ethics have been heavily influenced by racism, specifically through the false assumption of race as a biological difference rather than a social construct. Historical trauma has an impact across generations and has resulted in a high level of mistrust of patients toward clinicians. It is the responsibility of healthcare clinicians to understand the impact of structural racism and implicit bias as they relate to their own ethical decision-making.
Ethical decision-making as a clinician requires you to understand the
professional code of ethics you are accountable to, relevant legislation,
and the influence of history and tradition on the practice of medicine.
Accountability to a code of ethics is a key element of defining any profession.
Cruess et al. (2004) in their definition of "profession," emphasize that any
profession "must be governed by codes of ethics and profess a commitment to
competence, integrity and morality, altruism, and the promotion of the public
good within their domain. These commitments form the basis of a social contract
between a profession and society, which in return grants the profession a
monopoly over the use of its knowledge base, the right to considerable autonomy
in practice and the privilege of self-regulation. Professions and their members
are accountable to those served and to society." This social contract in the
medical profession is heavily influenced by both legislation and tradition.
You can see that your ability to adhere to the four principles of ethical
decision making in healthcare can be influenced by implicit and explicit
biases within a healthcare system that has been shaped by structural racism.
These principles are: beneficence (doing good), non-maleficence (doing no harm),
autonomy (giving the patient the freedom to choose freely, where they are able)
and justice (ensuring fairness in care.)
The impact of racism on medical ethics is well-documented. Medical research
has persistently maintained assumptions that there are physiologic and genetic
differences based on race, though it is proven that race is a social construct.
When medical researchers continue to search for false correlations between race
and disease, the more important focus on public health and the roles that social
determinants of health play in health outcomes for marginalized populations is
lost (Perez-Rodriguez, & de la Fuente, 2017). Research that begins with the
assumption of race as a biological rather than social construct leads to
inherently unethical and unequal treatment decisions. To maintain an ethical
social contract between you as the clinician and your patients, you must
critically evaluate your understanding of the impact of historical trauma
and unconscious bias. Your relationship with your patients must be informed
by your understanding of these concepts, as well as the roles that social
determinants of health may play in your treatment decisions and health
outcomes for your patients.
Key Point: Medical ethics has been heavily influenced by racism,
specifically through the false assumption of race as a biological difference
rather than a social construct.
Historical Trauma
Historical trauma is defined as the cumulative effect of
harm that spans generations and can impact both physical and emotional
wellbeing (Gameon & Skewes, 2020). Historical trauma is a barrier to full
access to healthcare for people of color. The history of exploitation of
people of color in the name of medical advancement and the resulting trauma
undermines the trust between patient and provider. You are most likely familiar
with many examples of unethical and traumatic medical mistreatment of Black
people in the United States. The Tuskegee Syphilis Study, conducted by the U.S.
Public Health Service, surgical experiments on Black women and the use of
cancer cells for research without consent represent just a few of the many
traumas inflicted upon Black people.
Access to healthcare was segregated from the beginning of the medical profession
in the United States. Racial disparities in the delivery of care were intentional
early in the history of medicine, and the result was consistently poor health
outcomes for Black people and a deep mistrust of the medical profession (Miller &
Miller, 2021). Patient/client trust in your care is essential for you to be
able to deliver care on an ethical foundation. Mistrust in science and in
healthcare clinicians is endemic in the U.S., as seen in vaccine hesitancy
and reluctance to participate in clinical trials. A number of studies
illustrate how the legacy of structural racism has generated mistrust in Black
communities that contribute to stark healthcare disparities (Powell, 2019; Warren,
2019; Warren, 2020).
Historical trauma is not limited to the experiences of Black people.
Asian American Pacific Islanders have also been subjected to racism and the
resulting negative impact on health outcomes. Japanese Americans were detained
in camps after the 1941 attack on Pearl Harbor. In subsequent studies on the
intergenerational impact of internment it was found that there were disparate
health outcomes for those who were detained in the camps, loss of family businesses
and a negative impact on mental health for future generations, as well as a
mistrust of the government (Patel & Nagata, 2021). In the 20th century, about
one third of women of childbearing age in Puerto Rico were coerced into becoming
sterilized. This was promoted and subsidized by the United States government
through Puerto Rican public health institutions (Lazare, 2021). In the 1940s,
U.S. Public Health Service researchers intentionally exposed over 1,300 sex
workers, soldiers, prisoners and psychiatric patients to sexually transmitted
diseases (STDs) without their consent to test the effectiveness of prophylactic
interventions (Spector‐Bagdady, 2019).
These experiences of historical trauma represent just a small portion of the
number of unique histories that people of color in the United States bring with
them into their healthcare encounters. It is important for you to consider the
possible impact of historical trauma on trust and confidence in your ability and
willingness to care for your patients. It is critical that you take concrete steps
to demonstrate that you understand the background, history and experiences of your
patients, their communities and their cultures. There are ways to build trust so
that you can work toward a more effective patient-physician relationship.
Explicitly acknowledging the history of racism in medicine and encouraging
patients to share their stories and their biases could lay the groundwork for
a more trusting relationship. Asking patients what they need from you to build
trust can also be a pathway to intentional conversations that will deepen the
patient-physician relationship (Miller & Miller, 2021). Finally, you can
continue to research and educate yourself on the complex intersection of the
history of racism and medicine as it relates to marginalized populations so
that you understand the perspective of these patients. Taking these steps
will help you to develop your trustworthiness as a physician as you work with
your patients toward better health outcomes.
Key Point: Historical trauma has an impact across generations and has
resulted in a high level of mistrust of patients toward physicians. There are
specific, intentional steps that you can take as a physician to mitigate the
impact of historical trauma and support the ethical practice of medicine.
The COVID-19 pandemic amplified the need for ethical decision-making in
medicine and further emphasized significant disparities in care for marginalized
communities. The convergence of poor health outcomes due to existing social
determinants of health and systemic disparities in access to care resulted
in more people of color who were disproportionately in need of hospitalization
due to the virus (Tochin et al., 2020). Once these patients arrived at the
hospital, triage protocols in place to manage limited resources further
disadvantaged people of color. Traditional methods of medical decision-making
in allocating scarce resources falsely assume a baseline measure of health and
do not take into account the impact of systemic racism and social determinants
of health on diverse patient populations (Schmidt et al., 2020). This is just
one example of many that represents the complexity of ethical decision-making
in healthcare and the persistent negative impact of structural racism in the
delivery of healthcare.
In a study examining disparities in the treatment of pain for Black and White
patients, researchers examined the beliefs of medical students and residents about
biological differences between the two patient groups (Hoffman et al., 2016).
The study concluded that medical students who endorsed the belief about
biological differences made unequal treatment decisions due to falsely held
beliefs about biological differences between Black and White patients
(Hoffman et al., 2016). In another study, Perez-Rodriguez and de la Fuente
(2017) examined the interpretation of research studies on the prevalence
of a particular form of breast cancer (TNBC) among Black women. The results
of the study were reported solely based on the race of the women but failed
to account for the fact that in each category of analysis, there was strong
evidence that socioeconomic status and Medicaid as the primary insurance
coverage were also significantly related to the presence of TNBC.
A study demonstrating how implicit bias can affect medical decision making
showed videos of patients complaining of symptoms suggestive of coronary artery
disease to 720 primary care physicians. The actors varied by age, race and gender
but told the exact same stories of their symptoms. They found that women
(odds ratio, 0.60; 95 percent confidence interval, 0.4 to 0.9; P=0.02) and
blacks (odds ratio, 0.60; 95 percent confidence interval, 0.4 to 0.9; P=0.02)
were less likely to be referred for cardiac catheterization than men and Whites
(Schuman et al., 1999). The book Unequal Treatment by the Institute of Medicine
documents the many ways that racial and ethnic disparities in healthcare are
significant predictors of the quality of healthcare, even after accounting for
the effects of socioeconomic conditions (Smedley, Stith, Nelson, 2003).
These examples emphasize that your responsibility as a clinician is to constantly
engage in critical self-reflection to ensure that your treatment decisions are
based on the individual factors for each patient and that your decisions are free
from racial bias. Because implicit bias can influence your decision-making, you
can seek objective input from other peers on a routine basis to ensure that
you are aware of any blind spots or concerning patterns in your treatment
decisions. Listen to your patients carefully and identify
support people to help advocate for patients, such as social workers,
community health workers, etc. Additional responsibility of the clinician
is to effectively communicate with patients regardless of their preferred
language. This includes effective use of professional interpretation services
and knowledge of institutional policies.
Commit to
continuing education to better understand the impact of implicit bias on
medical decision-making. Finally, you can actively advocate for changes to
the medical school curriculum that continues to teach that there are biological
differences between races. Williams et al. (2018) found that when medical
schools intentionally incorporate these concepts throughout their curriculum,
their students are less likely to demonstrate biased medical decision-making
behaviors.
Key Point: Structural racism has influenced the field of medicine and
continues to inform research and medical education. It is a false belief that
there are biological differences between races. It is the responsibility of
clinicians to understand the impact of structural racism and implicit bias as
they relate to their own ethical decision-making.
To ensure that your care is based on the ethical foundations of beneficence,
non-maleficence, autonomy and justice, you have an ethical responsibility to
understand the impact of structural racism on the practice of medicine. The
resulting historical trauma experienced by multiple marginalized people negatively
impacts the development of a trusting and effective patient-clinician relationship.
Your treatment decisions are influenced by your unexamined implicit biases. You are
responsible for actively working to build trust with your patients and for being aware
of your biases and how they may be impacting your treatment decisions. As a clinician
you have the capacity to challenge long held misconceptions in the
field of medicine that uphold racist practices.
R. Ellen Pearlman, MD, FACH
According to Delgado and Stefancic (2001), race-consciousness is explicit
acknowledgment of the workings of race and racism in social contexts or in
one's personal life. In healthcare, this means acknowledging that racial health
inequities are the result of racism, not the result of genetics. Applying
race-consciousness to healthcare requires:
• an appreciation of the complex historical journey
of Black people and/or persons of color;
• knowledge of disparities in health which
may facilitate or inhibit optimal levels of care for these individuals
and their families;
• and the self-appraisal of one's attitudes, feelings,
beliefs and biases towards Black people and/or persons of color (Watts, 2003).
Race-consciousness is often juxtaposed to colorblindness, which acknowledges
the arbitrary nature of race, yet ignores the inequities created as a result of
structural racism.
When we talk about having privilege, what exactly do we mean? A privilege is an unearned, mostly unacknowledged societal advantage (right, benefit, or immunity) that a restricted group of people has over another group. The nature of privilege in systems of oppression is that those who possess it are frequently unaware of it. Peggy McIntosh, in her seminal article, describes how "privilege is like an invisible weightless knapsack of special provisions, maps, passports, codebooks, visas, clothes, tools, and blank checks." She proceeds to write down examples from her daily life of "White" privilege that she has taken for granted. The following are excerpts from her list:
- If I should need to move, I can be pretty sure of renting or purchasing housing in an area which I can afford and in which I would want to live. I can be pretty sure that my neighbors in such a location will be neutral or pleasant to me.
- I can go shopping alone most of the time, pretty well assured that I will not be followed or harassed.
- I do not have to educate my children to be aware of systemic racism for their own daily physical protection.
- I can be pretty sure that if I ask to talk to the "person in charge," I will be facing a person of my race.
- If a traffic cop pulls me over or if the IRS audits my tax return, I can be sure I haven't been singled out because of my race.
- I have been taught since an early age that people of my own race can become doctors.
- Throughout my education, I could succeed academically without people questioning whether my accomplishments were attributable to affirmative action or my own abilities.
- When I applied to medical school, I could choose from many elite institutions that were founded to train inexperienced doctors of my race by "practicing" medicine on urban and poor people of color.
- I am reminded daily that my medical knowledge is based on the discoveries made by people who looked like me without being reminded that some of the most painful discoveries were made through inhumane and nonconsensual experimentation on people of color.
- When I walk into an exam room with a person of color, patients invariably assume I am the doctor in charge, even if the person of color is my attending.
- If I respond to a call for medical assistance on an airplane, people will assume I am really a physician because of my race.
- Every American hospital I have ever entered contained portraits of department chairs and hospital presidents who are physicians of my race, reminding me of my race’s importance since the founding of these institutions.
- Even if I forget my identification badge, I can walk into the hospital and know that security guards will probably not stop me because of the color of my skin.
- I have been taught since an early age that people of my own race can become doctors.
- Throughout my education, I could succeed academically without people questioning whether my accomplishments were attributable to affirmative action or my own abilities.
- When I applied to medical school, I could choose from many elite institutions that were founded to train inexperienced doctors of my race by "practicing" medicine on urban and poor people of color.
- I am reminded daily that my medical knowledge is based on the discoveries made by people who looked like me without being reminded that some of the most painful discoveries were made through inhumane and nonconsensual experimentation on people of color.
- When I walk into an exam room with a person of color, patients invariably assume I am the doctor in charge, even if the person of color is my attending.
- If I respond to a call for medical assistance on an airplane, people will assume I am really a physician because of my race.
- Every American hospital I have ever entered contained portraits of department chairs and hospital presidents who are physicians of my race, reminding me of my race’s importance since the founding of these institutions.
- Even if I forget my identification badge, I can walk into the hospital and know that security guards will probably not stop me because of the color of my skin.
She describes White fragility as "…a state in which even a minimum amount of racial stress becomes intolerable, triggering a range of defensive moves. These moves include the outward display of emotions such as anger, fear, and guilt, and behaviors such as argumentation, silence, and leaving the stress-inducing situation. These behaviors, in turn, function to reinstate White racial equilibrium" (DiAngelo, 2011).
The following table shows the typical emotional reactions, behaviors, and claims that White people make in conversations about race that indicate fragility.
| Emotional Reactions to Receiving Feedback about Bias | Behavioral Reactions to Receiving Feedback about Bias | Common Claims Made after Receiving Feedback about Bias |
|---|---|---|
Feeling…
|
Crying Physically leaving Emotionally withdrawing Arguing Denying Focusing on intentions Seeking absolution Avoiding |
"I know people of color." "You are judging me." "You are generalizing." "You’re playing the race card." "You’re being racist against me." "You are making me feel guilty." "You hurt my feelings." "The real oppression is class (or gender, or anything other than race)." "I don’t feel safe." "The problem is your tone." "That was not my intention." "I have suffered too." |
| The 11 Unspoken Rules of White Fragility | |
|---|---|
| 1 | "Do not give me feedback on my racism under any circumstances." This is a cardinal rule. However, if you break this rule, then make sure to follow the others. |
| 2 | "Proper tone is crucial - feedback must be given calmly. If any emotion is displayed, the feedback is invalid and can be dismissed." |
| 3 | "There must be trust between us. You must trust that I am in no way racist before you can give me feedback on my racism." |
| 4 | "Our relationship must be issue-free - if there are issues between us, you cannot give me feedback on racism until these unrelated issues are resolved." |
| 5 | "Feedback must be given immediately. If you wait too long, the feedback will be discounted because it was not given sooner." |
| 6 | "You must give feedback privately, regardless of whether the incident occurred in front of other people. To give feedback in front of any others who were involved in the situation is to commit a serious social transgression. If you cannot protect me from embarrassment, the feedback is invalid, and you are the transgressor." |
| 7 | "You must be as indirect as possible. Directness is insensitive and will invalidate the feedback and require repair." |
| 8 | "As a White person, I must feel completely safe during any discussion of race. Suggesting that I have racist assumptions or patterns will cause me to feel unsafe, so you will need to rebuild my trust by never giving me feedback again. Point of clarification: when I say "safe," what I really mean is "comfortable."" |
| 9 | "Highlighting my racial privilege invalidates the form of oppression that I experience (e.g. classism, sexism, heterosexism, ageism, ableism, transphobia.) We will then need to turn our attention to how you oppressed me." |
| 10 | "You must acknowledge my intentions (always good) and agree that my good intentions cancel out the impact of my behavior." |
| 11 | "To suggest my behavior had a racist impact is to have misunderstood me. You will need to allow me to explain myself until you can acknowledge that it was your misunderstanding." |
According to DiAngelo, White fragility serves the following functions; It:
- Maintains White solidarity,
- Closes off self-reflection,
- Trivializes the reality of racism,
- Silences the discussion,
- Makes White people the victims,
- Hijacks the conversation,
- Protects a limited worldview,
- Takes race off the table,
- Protects White privilege,
- Focuses on the messenger, not the message, and
- Rallies more resources to White people.
DiAngelo argues that in order to dismantle structural racism, White people will need to learn to tolerate discussions around race and racism without becoming defensive or apathetic. She suggests that White people learn to approach conversations about race with a growth mindset by consciously working to shift emotions, behaviors, and responses to engage in the conversation. See the table below for her suggestions:
| Reframe Your Emotions to Receiving Feedback | Behavioral Reactions to Receiving Feedback | Reframed Claims to Make in Response to Feedback |
|---|---|---|
Embrace…
|
Engage in…
|
State…
|
- Seeing White Fragility: https://www.youtube.com/watch?v=CdFCRHhygHo
Robin DiAngelo comments on her work in these videos:
The nature of racial conflict is introduced and contributing factors are discussed, especially in the context of healthcare. Racial conflict is inextricably linked to stereotypes, bias, privilege, discrimination, racism and inequities.
Racial conflict is a type of social conflict that results in threatened or actual
harm to the targeted racial group based on perceived racial differences. Outright
racism, oppression, discrimination, mistreatment, and offensive racist words and
actions underlie racial conflict. After learning key concepts of race, racism and
the history of racism in the U.S., it may be easier to grasp why racial conflict
exists. The stereotypical perception and treatment of an entire racial group as
"less than" inevitably results in grievances and eventually generates conflict
as disadvantaged groups challenge the status quo and compete for power and resources.
The additional context of the history of racism in healthcare (Hess et al., 2020),
specifically, reveals the grim reality of systemic racial inequities leading to
health and social disparities (Ricks et al., 2021; Sim et al., 2021). In the U.S.
today, we see how minoritized racial groups continue to suffer restricted access to
basic needs such as healthy foods, clean air and water, safe areas for exercise and
access to healthcare (Johnson-Agbakwu, 2022). These same marginalized populations
already face disparate health outcomes (Sim et al., 2021) and continue to be
subjected to race-based chronic stress due to generations of exposure to
discrimination and injustice.
Healthcare can be added to the list of resources for which minoritized racial
groups must compete. Certainly, White privilege and fragility play a large role
in maintaining a system that serves to sustain these inequities and serves to keep
White people from fully grasping the depth and breadth of the problem (Hess et al.,
2020). How can White people mitigate racial conflict? What are the processes and
pathways for moving away from inequity and toward empathy, understanding and
transformative change in healthcare (Hagiwara et al., 2019; Hess et al., 2020;
Sim et al., 2021) for Black people and people of color? It is imperative to reckon
with the historical racial discrimination and mistreatment, and to acknowledge
the disparities that lead to shortening people’s life span by 20 years, simply as
a function of their zip code. Trainees and healthcare professionals entering the
field must shine a light on the role of racial conflict in ongoing health inequities,
refuse to contribute to and/or sustain the distortions of racial bias and lead the
transformation to equitable healthcare.
Bias is defined and presented as the root of racism and unequal healthcare treatment. Neuropsychology explains how stereotypes and bias develop, and research has identified possible ways to measure and mitigate bias.
Biases are learned beliefs and attitudes about others that may be positive or
negative, like prejudice and stereotypes. Biases are formed early in life through
exposure to biased media, education and people, and they are often culturally
reinforced. Racialized medical theories from the 1850s that people of African
descent have a higher threshold of pain, still contribute to bias today and affect
medical practice. Studies show evaluation and treatment of pain for Black patients
compared to Whites was negatively impacted by medical students who endorsed this
racial bias. Racial bias is also closely linked to health inequities. Bias ranges
from subtle microaggressions to more overt episodes of major bias, and both can be
detrimental to health and well-being. Being targeted on a daily basis naturally
leads to heightened watchfulness or even vigilance, which has serious implications
for chronic stress and health. An APA article (2022) highlights vast disparities in
access to healthcare that were exposed by the COVID-19 pandemic. One serious outcome
is how people of color were hit harder by COVID-19 due to institutionalized racism.
Psychologists assert that racism is the root cause of unequal healthcare treatment,
policies and access in the U.S.
Black people and other non-White racial groups regularly face discrimination from
healthcare providers. Providers may be aware or conscious of some bias and unaware
of other aspects of bias (e.g., implicit bias). The human brain makes rapid and
automatic associations, naturally putting things in categories to make sense of
the world. Stereotyping is an automatic cognitive process of generalizing and
placing people in categories, which is more likely to occur under conditions of
stress. A stereotype is a generalization about a person or group of people without
regard to individual differences. Even stereotypes that seem positive may have
negative consequences.
Negative bias leading to mistreatment often stems from fear and misunderstanding of
difference. Whether implicit bias, prejudice or stereotypes, these attitudes affect
our understanding, actions and decisions. Since conscious and unconscious bias
involve learned stereotypes, values and behaviors, it is believed that they can
be unlearned and reduced through conscious attention. If you are a member of a
minoritized group, negative stereotypes can undermine your self-esteem. One popular
strategy for mitigating bias is to learn more about your own unconscious bias by
taking the Harvard Implicit Association Test
(IAT https://implicit.harvard.edu/implicit/),
raising self-awareness and applying
various strategies to become more conscious of how your biases may affect your
behavior, decisions, and self-esteem. By slowing things down, people are likely to
align their conscious beliefs, values and behaviors in more equitable treatment of
others.
To cultivate a more diverse workforce in healthcare and positively affect patient
outcomes and health equity, we must find ways to effectively intervene with our own
bias and associated behaviors. Sometimes a biased response may be avoided by naming
it, reflecting and replacing it with a more reasoned choice. Creating
counter-stereotypic images can help to challenge the validity of a stereotype.
Exposure to those who are different from oneself often provides specific information
about group members that can prevent stereotyping in the future. It also helps trying
on the perspective of others. Extensive research and discussion of these and other
interventions are discussed in Science of Equality article (2014) about addressing
implicit bias. Studies, such as Burke et al. (2017), are developing and testing new
strategies for addressing implicit bias, stereotypes and prejudices
held by providers.
Cultivating your emotional intelligence is essential to understanding the
experiences of racially minoritized individuals and countering your implicit
biases and stereotyping. Emotional intelligence is the ability to recognize your
own and other people's emotions, label them appropriately and use this understanding
in interpersonal relationships. It also involves the capacity to manage one's
emotions (Goleman, 1996). Perhaps the most important and practical aspect of this
concept is your ability to regulate your emotions. This is an essential skill in
clinical care and in life. This involves intentionally pausing for a few seconds
before you react emotionally, thinking about the likely reasons for the other
person's statement that triggered you, how they might react to your intended
reply and the consequences of that reaction. You may decide to react in a different,
more conciliatory or helpful way. You can explore your EQ (Emotional Quotient) by
taking a quick test at this website: https://www.ihhp.com/free-eq-quiz/
- A patient not being believed or taken seriously (Microinvalidation)
- A belief that a person of color couldn’t possibly occupy a high-status position, e.g., when a clinician is mistaken for a lower status role on a clinical team
- Ignoring the person of color in line at the pharmacy and serving the White people in line first (Sue, 2010)
- Stereotype threat or being at risk of confirming, as self-characteristic, a negative stereotype about one's group
- A peer White student says she doesn't see (person of color) as different – "I don’t see color!" - and points to similarities in class for her justification
Nixon, S.A. The coin model of privilege and critical allyship: implications for
health. BMC Public Health 19, 1637 (2019). https://doi.org/10.1186/s12889-019-7884-9
Overland MK, Zumsteg JM, Lindo EG, et al. (2019). Microaggressions in Clinical
Training and Practice. PM & R. 2019;11(9):1004-1012. doi:10.1002/pmrj.12229
Steele, Claude M. (2010). Whistling Vivaldi: How stereotypes affect us and what we
can do. New York: W.W. Norton & Company, Inc.
Medical Student and Medical Trainee Change studies: https://www.diversityscience.org/changes/
When cultures collide, the only minimal chance for a partnership that values diversity is when one side is open-minded to understanding differences and demonstrates flexible behaviors. Positive outcomes of valuing diversity include improved communication, satisfaction, empowerment, partnerships, respect, optimal care, health and wellness.
Introduction
Leaders in various disciplines are increasingly realizing the importance of recognizing
diversity and applying cultural humility for successful outcomes. The concept of diversity
is vastly broad, including cultural differences that span from differences in beliefs
among nations, communities and groups to diversity at the individual level—including
diversity of thought. When a difference in perspective is misunderstood or not
adequately considered, the resulting conflict interferes with accomplishment of
goals and relationships. To guide healthcare professionals on how to appreciate
diversity and apply cultural humility to advance mutual understanding and
improve human interactions is the intent.
Cultural Humility Definition
Tervalon and Murray-Garcia (1998) coined the term cultural humility. In a seminal article
describing multicultural training to physicians, they encouraged educators to shift away
from the goal of achieving cultural competence to that of cultural humility. "Cultural
humility incorporates a lifelong commitment to self-evaluation and self-critique, to
redressing the power imbalances in the patient-physician dynamic, and to developing
mutually beneficial and non-paternalistic clinical and advocacy partnerships with communities
on behalf of individuals and defined populations." (Tervalon & Murray-Garcia, 1998, p. 117)
While both cultural competency and cultural humility involve a process, cultural humility
is a process of lifelong learning.
Attributes of Cultural Humility
Attributes of cultural humility include addressing power differences and
recognizing and minimizing power differences, promoting respect, focusing on not
only the other individual but on yourself, being flexible, making bias explicit
and adopting an ongoing process of self-reflection and growth in your appreciation
of and ability to be enriched by differences (Yeager & Bauer-Wu, 2013). Flexibility
is an endpoint and an attribute of cultural humility. The attributes were openness,
self-awareness, egoless, supportive interactions, and self-reflection and critique.
The outcomes were mutual empowerment, partnerships, respect, optimal care and
lifelong learning.
Behaviors to Adopt Cultural Humility and Value Diversity
Enacting cultural humility involves a flexible mindset, a
focus on others and self (as opposed to self only) and a
perspective that the worth of all humans is on a horizontal
plane, meaning that all human beings hold equal value and
diversity is valued. Cultural humility involves supportive
interactions, which may include verbal and/or nonverbal
communications. Cultural humility is a process of self-reflection
and lifelong learning resulting in mutually positive outcomes.
In practice, cultural humility is expressed by being curious
about cultural beliefs and how they impact attitudes and
behaviors and expressing empathy and respect for
patients/clients' choices influenced by their cultural
beliefs. (Chou, Pearlman, Risdon. 2014) If you are aware
of your biases and stereotyping, you can step away from
these, and work on not letting them interfere with your
generous listening in the service of understanding your
patients and clients.
To align cultural humility and diversity the following assumptions must be understood:
- All humans are diverse from each other in some way yet part of a global community.
- Humans are inherently altruistic.
- All humans have equal value.
- Cultural conflict is a normal and expected part of life.
- All humans are lifelong learners.
Conclusion
To thrive in a diverse, complex world, individual, group leaders or community
leaders need to be able to embrace cultural humility. By being aware of diversity
and power imbalances that affect perspective, conflict can be accepted and embraced
in a positive way. By enacting behaviors that demonstrate cultural humility, mutual
benefits result. When cultures collide, the only minimal chance for a partnership
that values diversity is when one side is open-minded to understanding differences
and demonstrates flexible behaviors. Positive outcomes include improved communication,
satisfaction, empowerment, partnerships, respect, optimal care, health and wellness.
Approaching diversity as positive and not centered on conflict, you will reinforce
behaviors that flatten hierarchies, better value humankind and role model flexibility
to resolve conflict positively. Diversity represented by sociocultural differences can
affect communication and decision making and are directly linked to patient satisfaction,
treatment plan adherence and overall care quality.
Microaggression is defined and explored in the context of healthcare. The harm and long-term consequences are discussed, including impact on a target's safety and their psychological and physical health.
In the 1970s, Harvard professor Dr. Chester M. Pierce coined the term
"microaggression" to describe the insults and slights he had witnessed against
Black people, noting the pervasive effect of multiple microaggressions by White
people. Microaggressions are defined as verbal, nonverbal and/or environmental
slights, snubs or insults that are either intentional or unintentional. They convey
hostile, derogatory or otherwise negative messages to target persons based upon their
membership in a structurally oppressed social group (Sue, 2010).
Individual microaggressions may appear small or insignificant, but part of the harm
is the day-to-day accumulation of being targeted repetitively in a variety of
different contexts over time. While a White person might see their microaggression
as an honest mistake that should be shrugged off, someone who is structurally
oppressed is more likely to experience microaggressions repeatedly, beyond a
healthcare context, and to be more severely impacted (Freeman & Stewart, 2018).
Overland, Zumsteg, Lindo, Sholas, Montenegro et al. (2019) encourage practitioners
to focus on the impact of microaggressions and their effect on the target rather
than on defending one’s intentions or saying what the actor meant by the behavior.
A common response after committing a microaggression is to frame it as a joke, which
invokes another microaggression (invalidating the impact on the target).
Microaggressions may be committed without racist intent, but perpetrators of the
microaggressions often do not take responsibility for how their words
might be landing. Only people of color are able to truly discern what constitutes
a derogatory message or microaggression. Overland et al. (2019) also cite barriers
to recruitment and retention of high-quality candidates as powerful reasons to
change a culture permeated by microaggressions that demean and degrade physicians
of color. The ripple effect of fewer practitioners of color is poorer patient
care and outcomes, and greater healthcare disparities.
Microaggressions are committed by health providers against patients and trainees, by patients against clinicians,
and they also occur on interprofessional teams and between colleagues. Microaggressions undermine these relationships,
diminishing trust and affecting the care that can be provided. Stereotypes have led clinicians to overlook symptoms or
not take a patient seriously. Some of the harmful consequences for people of color encountering recurrent discrimination
by healthcare providers include added stress, distrust of healthcare practitioners, skepticism, and related delays in seeking
medical care and following up, and not adhering to prescribed treatments or screening recommendations (Sabin et al., 2009).
It is important to be familiar with a range of marginalized and privileged social
identities to understand how microaggressions might occur. it may be difficult to
have empathy for those who are marginalized by the very privilege that one holds.
Gaining exposure to the lived experiences of those who are targeted by racism takes
intentional work and practice. Culture can be shifted by owning and understanding
one’s own bias and microaggressions. Freeman and Stewart (2018) recommend that
healthcare providers commit to understanding and recognizing microaggressions,
the severity of resulting harm and be mindful to prevent committing microaggressions.
See Cheung et al. (2016) for their protocol for targets and witnesses to take
A.C.T.I.O.N. in responding to microaggressions: Ask about the intentions of the
microaggressor ("I want to make sure I understand what you were saying. Were you
saying...?"); Come from Curiosity instead of judgment, listening carefully;
Tell
others how the microaggression was problematic ("I noticed that…."); focus on the
Impact, asking for or stating the potential impact of such a statement or action
on others; Own your thoughts/feelings (When I hear your comment,
I think/feel..."); discuss Next steps, requesting that appropriate action
be taken and checking in with the target of the microaggression.
- "I want to be treated by an American doctor."
- Even a supposed compliment can be derogatory: "You’re so articulate," said to a person of color reflects the underlying belief that people of color are generally not as intelligent as White people.
- Gaslighting for women of color - (Freeman and Stewart, 2018). Stern describes the invalidating experience of being "gaslit" as "soul destroying" and argues that women whose feelings are frequently invalidated in this way often start to second guess their ability to make decisions for themselves or conclude that their concerns aren’t worth articulating at all. In this way, emotional microaggressions that invalidate women’s emotional responses to their illnesses and dismiss their physical symptoms can result in enduring harms.
- Microaggressions in clinical training and practice (Overland et al., 2019). A student’s example - I have been asked so many times about where I am from based on my ethnicity, that I am just used to it.
- "Most White providers, for example, are not routinely asked, ‘Where are you really from?’ or ‘Did you train in the United States?’ They are typically not complimented with ‘You speak English really well’ or ‘You are very articulate.’ White providers may not be as frequently asked to ‘smile more,’ ‘soften their tone’ or to ‘not sound so authoritative,’ because others perceive them as being ‘angry’ or ‘intimidating and unsafe to approach.’ Because Whiteness, masculinity and the role of a physician are attributed disproportionate value in our culture, it is not surprising that White male providers are rarely asked ‘Can I please see the doctor now?’" (Overland et al., 2019)
- Belief that everyone can succeed if they work hard enough assumes: The playing field is even so if people of color don’t get the job, the problem lies with them.
Banaji, M. R. and Greenwald, A. G. (2013). Blindspot: Hidden Biases of Good People.
New York: Delacorte Press.
Jana, T., & Baran, M. (2020). Subtle Acts of Exclusion: How to Understand,
Identify, and Stop Microaggressions. Oakland: Berrett-Koehler Publishers,
Incorporated.
https://ebookcentral.proquest.com/lib/vcu/detail.action?pq-origsite=primo&docID=6037198
Tweedy D. (2015). Black Man in a White Coat: a Doctor’s Reflections on Race and
Medicine. New York: Picador.
Washington, E. F., Birch, A. H., & Roberts, L. M. (2020, July 3). When and how to
respond to microaggressions. Harvard Business Review.
https://hbr.org/2020/07/when-and-how-to-respond-to-microaggressions
Janice H. Altman, PhD
In this section, you will learn about what discrimination is, some examples of racial discrimination throughout history, the impacts it can have on health and how it is a systemic issue.
Discrimination is the practice of unfairly treating a person or group of people differently
from other people or groups of people. Discrimination is behavior, arising from shared
cultural stereotypes and other mistaken beliefs about groups of people based on one aspect
of their social identity, such as race, age or gender. Sexism, for example, is a form of
discrimination based on a person's sex or gender that has been linked to stereotypes,
expectations and gender roles. Sex discrimination may include the belief that one sex
or gender is intrinsically superior to another. Extreme examples of sexism include sexual
harassment, rape and sexual violence. Ableism favors non-disabled people and treats them
as the standard of "normal living" while excluding and discriminating against people with
disabilities. Stereotypes or prejudice can be positive as well as negative. Prejudice
(similar to bias) means to prejudge a person or group of people; to have an opinion or
make a decision based on insufficient information.
Racial discrimination is when this unfair treatment is based on the perceived race of the person
or people. Amnesty International (2021) suggests that discrimination can come in different
forms. They present three different types of discrimination: direct, indirect and intersectional.
Direct discrimination is when there is an explicit distinction made between groups of people
where some individuals are less able than others to exercise their rights. Indirect
discrimination is when a policy or practice uses neutral terms, but disproportionately
disadvantages a specific group or groups. Finally, intersectional discrimination is
when several forms of discrimination combine to leave a group at an even larger
disadvantage than others.
Racial discrimination or racism in the U.S. is discrimination based on skin color.
Minoritized groups have historically had less access to privileges enjoyed by others, and the
impact of unequal access and treatment has cumulative consequences. Racial discrimination
in the field of healthcare includes historical and ongoing racially exploitative medical
and public health practices; failing to take symptoms seriously, dismissing severity of
pain and misdiagnosing illnesses (resulting in delayed treatment, unnecessarily advanced
disease states and increased hospitalizations or death due to heart disease or cancer).
This harm can be exacerbated for Black women, for example, when gender discrimination
is layered on top of racial discrimination.
Discrimination affects not only those who self-identify or are categorized as being members
of minoritized racial/ethnic groups but also harms those who are merely perceived by others
as belonging to these minoritized groups. For example, in one study MacIntosh et al. (2013)
noted in their discussion that U.S. adults who "self-identify as racial/ethnic minorities,
but report being socially-assigned as non-Hispanic White," reported better healthcare
outcomes and were less likely to report healthcare discrimination compared with those who
were perceived as racial/ethnic minorities.
The United States has a long history of engaging in racial discrimination.
Black people were enslaved in the United States from 1619 until the ratification of
the 13th amendment in 1865 (Shah & Adolphe, 2019). In 1830, President Andrew Jackson
signed the Indian Removal Act which authorized the forced relocation of thousands of
Native American people west of the Mississippi (Indian Removal Act, 1830). In the
late 19th century, Native American boarding schools were established in an effort
to assimilate Indigenous youth to American culture and eradicate Indigenous
cultures (Mejia, 2021). In 1882, the Chinese Exclusion Act suspended Chinese
immigration to the United States and made it impossible for Chinese
immigrants to apply for naturalization (History.com, 2018).
These are just a few examples of racial discrimination throughout U.S. history. You are
encouraged to conduct further research on these instances and the many other
examples of racial discrimination. It is essential to learn about the history
of racial discrimination because of the impacts and implications it has on
modern day society. In Sociological Perspectives on Racial Discrimination,
the authors discuss the discriminatory housing practice of redlining and state
that "though redlining eventually became illegal, the long-term consequences
of these and other obstacles to homeownership for the black-white wealth gap,
and for socioeconomic inequality more generally, surely lasted much longer"
(Small & Pager, 2020, p. 56). Being aware of racial discrimination throughout
history allows us to understand the implications of these practices. (Watch
video on how redlining causes inequality from previous
section: https://www.youtube.com/watch?v=O5FBJyqfoLM )
Many studies show that increased levels of perceived discrimination are associated with more negative mental and physical health. (Pascoe & Richman, 2009; Sabin et al., 2009) It is generally believed that racial discrimination causes stress, which has been shown to increase blood pressure, negatively impact sleep and raise the risk of developing kidney disease (Lewsley & White, 2020). It has also been found that people who said they had experienced racial discrimination were also cited as experiencing depression, anxiety, PTSD and other emotional distress (Lewsley & White, 2020). Studies that relate racial discrimination to negative impacts on physical and mental health suggest that racism and racial discrimination are a matter of public health. It is essential for incoming and current healthcare providers and researchers to become familiar with how real and perceived racial and ethnic differences can influence health outcomes (Nieblas-Bedolla et al., 2020).
It is important to note that discrimination is not simply an act that one person does to another, it is a system within our society. As you learned about in the "racial discrimination throughout U.S. history" section, discriminatory practices have been prevalent for centuries and undoing the negative implications of this history will take time. Due to historical and present-day racism, discrimination can be found throughout different arenas such as education, housing, medical treatment and the law. Discrimination works as a system, with discrimination in each institution potentially reinforcing disparities and discrimination in other institutions—and with the effects in some cases potentially reaching across generations (Lang & Kahn-Lang Spitzer, 2020). Although there is not one good answer on how to solve the issue of systemic discrimination, it is important to be aware of it if changes are going to be made.
- Avoidance of members of the target group - a racist patient who refuses to see a doctor of a minoritized racial/ethnic group
- Derogatory words or terms used to describe or refer to people of color
- Violating human rights of people of color, withholding access to healthcare, perpetuating inequality and inequities
Janice Thomas John DO, MS, MPH
Brooke Salzman, MD
This section defines health and healthcare equities, inequities and disparities, social and structural determinants of health, and racism as a determinant of health. We also examine how each of five social determinants likely impact overall health and explains how lack of access to oral health contributes to health disparities.
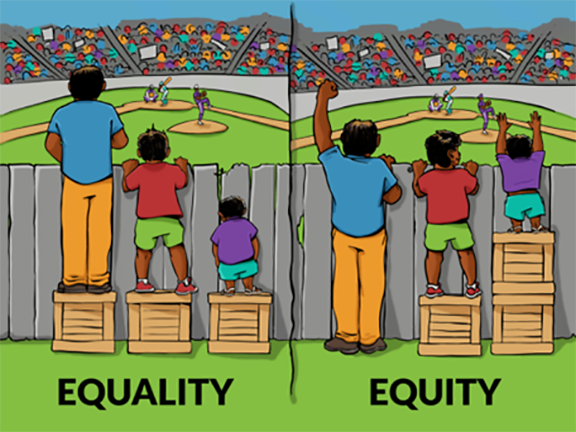
Interaction Institute for Social Change | Artist: Angus Maguire. https://interactioninstitute.org and http://madewithangus.com/
The World Health Organizations defines health as "a state of complete physical, social and mental well-being" (WHO).
Health Equity as defined by the Robert Wood Johnson Foundation (RWJF) "means that everyone has a fair and just opportunity to be as healthy as possible. This requires removing obstacles to health, such as poverty, discrimination and their consequences, including powerlessness and lack of access to good jobs with fair pay, quality education and housing, safe environments, and health care" (RWJF).
Health Inequity is therefore a difference in health that is avoidable and unfair because it is connected to social injustices and structural racism. These social injustices, due to an unequal allocation of power and resources, make some communities more susceptible to poor health compared to others. Examples include differences in life expectancies, mental illness diagnoses and preventable deaths. As an example, Black/African American, American Indian and Alaska Native women are two to three times more likely to die from pregnancy-related causes than White women. This is not due to any biological reason and in fact, crosses socioeconomic boundaries. If one racial or ethnic group can access a high level of medical care, why not others?
Health Disparities are connected to health inequities as the differences in the presence of disease and treatment outcomes between different population groups and communities. There is a higher degree of illness, injury or mortality in one group relative to another. Health disparities are inextricably linked to access to care, health insurance coverage, quality of care and use of care. When there is health inequity, health disparities emerge.
Healthcare Equity means that everyone has access to fair and appropriate care regardless of who they are, where they live or their socioeconomic status. This means that everyone has the same opportunity to be healthy. Everyone receives the quality of care appropriate for their needs.
Healthcare Disparities refer to the differences in healthcare between groups such as in health insurance coverage, access to and use of care, and quality of care. These disparities are usually discussed in terms of race and ethnicity, but can also be influenced by gender, socioeconomic status and sexual orientation, to name a few. The Affordable Care Act sought to address healthcare disparities by addressing the uninsured status across groups and the barriers to accessing healthcare.
Social Determinants of Health refer to the circumstances of the settings in which persons live, work, play, worship, attend school and grow old, that affect health, quality of life outcomes and risks (DHHS). They include five domains:
- Economic Stability
- Education Access and Quality
- Healthcare Access and Quality
- Neighborhood and Built Environment
- Social and Community Context
Structural Determinants of Health include the governing process, economic and social policies that affect pay, working conditions, housing and education. The structural determinants affect whether the resources necessary for health are distributed equally in society or whether they are unjustly distributed according to race, gender, socio-economic status, social class, geography, sexual identity or other socially defined group of people (NAS, 2017).
Racism as a Determinant of Health: Racism impacts overall health in various ways. In each social determinant there is an element that is affected by systemic racism. (1) A neighborhood or built environment with reduced access to healthy food, employment, housing and education and/or increased exposure to risk factors (e.g., avoidable contact with police); (2) Healthcare access diminished and adverse mental, social, emotional processes and associated psychopathology; (3) A lack of stability and quality healthcare, exposure to toxic facilities, fast food restaurants and alcohol outlets, connected to cumulative burden of life stresses and associated pathophysiological processes; (4) Lacking safe neighborhood and community spaces resulting in diminished participation in healthy behaviors (e.g., sleep and exercise) and/or increased engagement in unhealthy behaviors (e.g., alcohol consumption) either directly as stress coping or indirectly via reduced self-regulation; and (5) physical injury as a result of racially-motivated violence (Paradies et al., 2015).
In 2020, we witnessed the desolate collision of the social determinants of health, health disparities and access to care, as Native Americans, Black and Latinx communities faced much higher risk of COVID-19 infection (Johnson, 2020). This is not because their bodies were less able to fight the virus. Instead, health inequities made it more likely that they would be exposed to the virus and more easily infected. They were more likely to be working in the jobs that were considered essential, therefore exposed to more people and when they became infected, became more seriously ill. Lack of trust in their White healthcare providers, lack of insurance, lack of time and lack of access, also contributed to a higher likelihood of preexisting untreated chronic condition(s) that resulted in a reduced ability to fight the virus.
There are disparities in oral health that contributes to overall health disparities and must be addressed when considering the Social Determinants of Health (SDOH). Over time dental health providers have become a critical part of the healthcare team, and cannot only recognize the first signs of underlying systemic diseases found in the oral cavity, but address these factors with at-risk patients, as well as work to improve oral health (Tiwari, Palatta & Stewart, 2020).
Janice Thomas John, DO, MS, MPH
Brooke Salzman, MD
The pervasive impact of racism is systemic in its deepest and broadest roots. Therefore, to achieve racial equity we must explore and address oppressive policies, procedures and practices. Medical and scientific research which informs healthcare policies, procedures and practices must be intentional to use an inclusive approach that promotes health equity.
Structural racism can be described as the systemic oppression of certain ethnic and racial groups imposed by and embedded in laws, policies, procedures and practices in society. According to Kendi, "racism itself is institutional, structural, and systemic." Therefore, the antidote to this form of injustice is in making and enforcing changes to laws, policies, procedures and practices in society – one organization, one institution, one healthcare system, one community at a time.
Scholars have suggested the need for consistent definitions and accurate vocabulary for measuring, studying and discussing race, racism and health in healthcare organizations (Hardeman et al., 2016). Structural competency has been defined as "the capacity for health professionals to recognize and respond to health and illness as the downstream effects of broad social, political, and economic structures" (Neff et al., 2020). Health professionals need to consider not just the interpersonal strategies required to address overt racism in healthcare environments, but also the structural forces (laws, policies, procedures and practices) that shape the context in which they are embedded. Leaders of healthcare organizations must work to promote workforce inclusion and diversity in a way that addresses structural racism and how this may impact healthcare providers of color and the working environment.
- Examine our own backgrounds and biases.
- Commit to digging deeper into the data.
- Recognize that the research process itself impacts people and communities; researchers play a role in ensuring that research benefits communities.
- Engage communities as partners in research and credit them for their contributions.
- Guard against the implied or explicit assumption that White is the normative, standard or default position.
Racial and ethnic minorities continue to receive lower quality care and suffer higher rates of morbidity and mortality despite advances made in the treatment of chronic diseases. The reasons for these continued health disparities are rooted in social injustices and the structural racism that continues to plague communities of color. Scientists have known for years of the lack of a genetic component of race. The racial categories recognized in society have no basis at the genetic level. With that we say it is a "social construct"; this means it does not exist objectively but because human beings decided that it exists. Despite proof that the concept of race is "biological fiction" it continues to be used in medical teaching, treatment and research.
Recently, the term "race norming" and its use in medicine has been in the national news, due in
part to the way the NFL has compensated athletes suffering the effects of sports-related brain
injuries. Race norming is the adjustment of medical test results or medical risk assessments
based on a patient’s race. In other words, if you are Black, you might score differently than
you would if you are White with the identical or similar set of symptoms simply because of
the color of your skin.
The use of race-based norms embeds a number of assumptions about biological constructions
of race that may potentially lead to erroneous and potentially harmful interpretations
of racial differences. Further, the utilization of such norms not only reinforces
biological constructions of race but fails to question or understand why such differences
do exist. Efforts to improve equity in research need to include diverse populations
that reflect the composition of the U.S. and examine the underlying factors that may
lead to racial differences in health outcomes (Vyas, 2020).
Despite evidence that race is a social construct and has no genetic or biological basis, and
that genetic studies consistently show that there are more differences within racial groups
than between them, race-based protocols currently exist in medicine and can have a profound
impact on perpetuating racial inequities. An example includes assessments of kidney function
with equations that calculate estimated glomerular filtration rate (eGFR) such as the MDRD
equation. This equation includes inputs based on race. If a patient is identified as Black,
the MDRD will report a higher eGFR value, suggesting better kidney function. Higher eGFR
values have significant influence on subsequent care such as decisions to utilize certain
medications, referrals to specialist care, and meeting qualifications to be added to the
list for kidney transplantation. As a result, inputs to the eGFR equation based on race
amplify well known disparities in care such as White persons being at least four times
more likely to receive a kidney transplant than Black persons.
Janice Thomas John, DO, MS, MPH
Brooke Salzman, MD
- Admit to being a racist to become antiracist: Clinicians are more likely to do harm when they deny their racial biases.
- Slow down: Pause to heighten racial consciousness and prepare to challenge racism.
- Name and Identify racism first to challenge it: Diagnosis determines treatment.
- Learn the legacy of racism in American medicine (and beyond) to avoid perpetuating it.
- First do not harm: Prevent the toxic exposure of racism in the clinical encounter.
Antiracist approaches to clinical care begin with racial and ethnic representation. Increasing diversity in the healthcare workforce is accepted as an effective strategy for addressing access to care and health disparities in vulnerable populations. Documented increases in under-represented minority and disadvantaged graduates of healthcare professions have not kept pace with an ever-increasing diverse nation. Ethnic and racial diversity among dentists also does not mirror that of the U.S. population. In an increasingly diverse population, healthcare and public health workers are introduced to a broad spectrum of beliefs and various health related behaviors that are a result of different cultures.
More recently, there has been a shift from cultural competence to cultural humility as "competence" implies an endpoint for mastery. The cultural humility framework, instead, recognizes that we can never be fully competent in understanding all cultures and appreciates that culture is dynamic, changing over time and by location. The cultural humility framework embraces a growth mindset, self-reflection, and lifelong learning where individuals are open to learning about another’s culture and also examine one’s own cultural beliefs and identities.
Public health physician Melanie Tervalon and Dr. Murray-García (1998) described three principles of cultural humility: 1) Continue learning throughout our lives, because we are ever-changing based on what is going on with us and with our patients; 2) Be humble about our level of knowledge regarding our patients' beliefs and values, aware of our own assumptions and prejudices, and active in redressing the imbalance of power inherent in the clinician-patient relationship; and 3) Recognize the importance of institutional accountability.
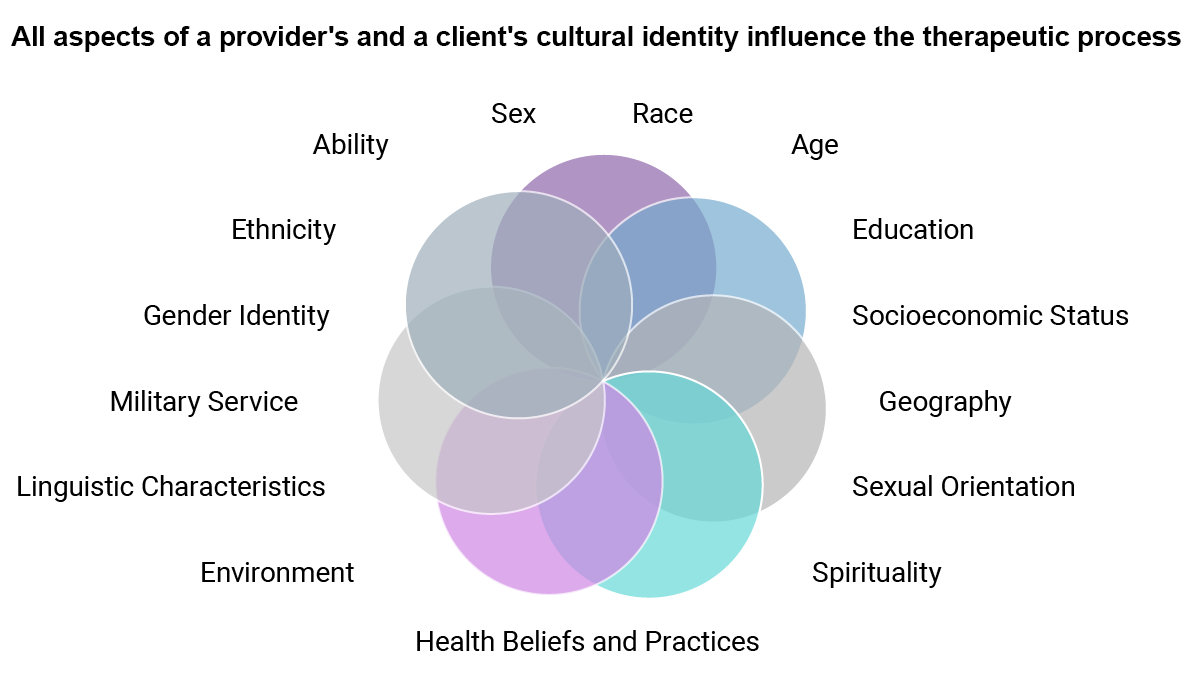
Core competencies in interprofessional collaborative practice (ICP) can provide a useful framework for guiding teams to address issues of racism and social justice in practice. These core competencies include:
- Work with individuals of other professions to maintain a climate of mutual respect and shared values.
- Use the knowledge of one’s own role and those of other professions to appropriately assess and address the healthcare needs of patients and to promote and advance the health of populations.
- Communicate with patients, families, communities and professionals in health and other fields in a responsive and responsible manner that supports a team approach to the promotion and maintenance of health and the prevention and treatment of disease.
- Apply relationship-building values and the principles of team dynamics to perform effectively in different team roles to plan, deliver, and evaluate patient/population-centered care and population health programs and policies that are safe, timely, efficient, effective and equitable.
Not infrequently, healthcare providers of color are subject to overtly racist behaviors
by patients which can lead to significant emotional harm. The profound harm is not merely
generated by the overt racist behaviors themselves but intensified by the failure of
organizations to respond to such acts, thereby neglecting to acknowledge their impact
on the workplace environment and provision of healthcare. Scholars have brought attention
to the dearth of policies and protocols that guide organizations on how to respond to
racism in healthcare settings despite its common occurrence; how to balance ethical
dilemmas involving the duty to provide care with the intention of creating a
nondiscriminatory environment. While many organizations have issued nondiscriminatory
proclamations and diversity statements, there needs to be a more substantive approach
to delineating, implementing, and evaluating the impact of anti-racist policies on
healthcare disparities, healthcare delivery, and the healthcare environment with
consideration given to guiding ethical principles, legal frameworks, and organizational
responsibilities.
Paul-Emile and colleagues (2016) outline a sequential approach to responding to racist
patients that preserves appropriate patient care and the well-being of physicians who
are the objects of racist (or sexist, homophobic, etc.) comments. Also, Dr. Holly
Humphrey, President of the Josiah Macy Jr. Foundation discusses an approach more
comprehensively in one of the Vital Voices podcasts of
the Foundation: https://macyfoundation.org/news-and-commentary/vital-voices-episode-4
Watch the videos in Discussion Question 23 to generate your discussion on approaching a racist patient.
Archana A. Pathak, PhD
R. Ellen Pearlman, MD, FACH
Allies are "people who recognize the unearned privilege they receive from society’s patterns of injustice and take responsibility for changing those patterns" (Bishop, 2015).
According to Brown and Osrove (2013), there are two factors that are highly correlated with allyship:
- Affirmation, that is communicating liking, caring and respect
- Informed action, that is demonstrating a willingness to be active on racial issues
- a "friend" –who may be high on affirmation but not on informed action; and
- an "activist," who may be an informed actor but not necessarily affirming.
When men suggested that sexism had taken place, targets of sexism
- reported increased self-confidence
- showed less stereotype confirmation and
- were more likely to file a complaint.
Performative allyship is when those with power/privilege profess solidarity with a cause, often to distance themselves from potential scrutiny or protect an institution brand (at the organizational level), or to get a virtual "pat on the back." It is "talking the talk" but not "walking the walk" (Medium, 2020).
L - listen and learn from the oppressed
L - leverage your privilege
Y - yield the floor
Allyship involves speaking up! It is often difficult to speak up to superiors, especially those who might evaluate you. Still, you have a voice, and if you do not use it, you become complicit in affirming a learning culture where bias is acceptable. Leila Hilal, MD, was a fourth-year student at Drexel University in January of 2022 when she told us this story:
The following sequence of videos is based on a story told to us by a Black woman medical student: She was on a trauma service when two Black teenagers were brought into the ER. One died immediately and the other was bleeding profusely. The trauma team stabilized him and were moving him to the OR, with the sounds of the teens’ families loudly crying in the waiting room. There were two White nurses and one White resident around the gurney, in addition to the Black woman student. One of the nurses said, "I’ll bet these boys didn’t do anything to deserve getting shot! They were probably on their way to church!"
The Black woman student was shocked and deeply saddened to hear that comment, but said nothing, since all efforts were focused on keeping the young man alive. Later she decided to say nothing, since she was afraid the trauma nurse might report her, resulting in a lowered grade. She instead brought the story to her professional formation small group. In our re-creation of this incident, we imagined a different ending to the story, involving allyship. We also highlight the various ways incidents like this can affect every member of a team. The actors in these videos, with the exception of an actor playing the nurse, were all medical students at Drexel University College of Medicine, who used their own thoughts and feelings to respond to this incident. They worked as a team to develop these videos.
We hired an actor to play the nurse who made the racist remark. She told us it was very difficult for her to play this role. She explained why:
Make the "Invisible" Visible
- Make the meta-communication explicit
- Ask for clarification
- Challenge the stereotype
Disarm the Microaggression/Macroaggression
- Develop rapport (acknowledging positive attributes)
- Describe what happened
- Express disagreement
- Interrupt and redirect
Educate the Offender
- Point out the commonality
- Appeal to the offender’s values and principles
- Differentiate between intent and impact
- Promote empathy
- Point to how they benefit
Speaking up can be challenging. You may feel like you are the junior person on a team. You may feel that it’s not your job to have a conversation with a superior or even a peer. You may worry about your evaluation. These are real concerns, and there are often confidential reporting systems that can address a team member who regularly makes racist or other biased comments. But every time a biased comment is met with silence, it becomes more acceptable to make these comments. It can poison a learning environment.
There are skills and approaches that can help you speak up effectively. Even if you are a junior person on your team and don’t feel empowered in the moment, it will help to learn and practice these skills, because in only a few years you will be a team leader, and it will be important to ensure that your learners work within a context of acceptance and respect for all.
This brief TED talk by Loretta Ross suggests a positive way to approach those who make racist and otherwise unprofessional comments: https://www.ted.com/talks/loretta_j_ross_don_t_call_people_out_call_them_in
Erica Riddick
We asked her if she would describe her experience of this exercise, and we are grateful for her reply: "This experience was both enlightening and cathartic for me as a minority student in medicine. Oftentimes, I find myself in the midst of challenging situations such as these but am hesitant to share my thoughts for fear that the other person may not understand my perspective. I appreciated this discussion as it enabled me to debunk common stereotypes about minority communities. This experience has encouraged me to use my voice unapologetically when faced with similar circumstances in the future."
It is important to set expectations when meeting with a team at the onset of a rotation. House staff, students and others need to know where and when to meet, what’s expected of presentations about patients and brief learning issues, bedside rounds etc.
Attendings should also say something about the learning climate that the team co-creates, for example, putting patients first, asking questions when you don’t know something, when and how to request a consult, etc. It is also important to discuss creating an environment that is respectful and inclusive for all. Below is an example of Dr. Novack beginning to set expectations, and a segue to a brief discussion about creating a bias-free learning environment.
There are particular opportunities in the care of our patients for interrupting and repairing inequities. To identify and understand those opportunities, it is useful to briefly review some core concepts:
- Financial security
- Nutritious food
- Education
- Safe housing
- Protection from environmental toxins
- Social support
- Social inclusion
Social privilege is an additional, key determinant of health. Decades of research have shown that social privilege and social power are health protective while social oppression results in poor health outcomes. Wealth is only one form of social privilege, a term that refers to a wide range of advantages some people get to enjoy based on their identity and at the expense of other people. Privilege means greater opportunities for income, education, housing, legal protections, social status, and advancement. In the U.S., historically privileged social identities include among others: White, male gender, cis-heterosexual, and able-bodied.
At every level of income, people who suffer social disadvantage or oppression have poorer health outcomes. BIPOC members of our communities are also more likely to suffer poverty, exclusion from educational and work opportunities, and social segregation or marginalization.
ZNA vs DNA. The zip code where you grow up – your ZNA – is a far more powerful determinant of health than DNA in predicting disease, disability, and life expectancy. Because of redlining, which placed affordable and healthy housing out of reach, and social segregation in the U.S., BIPOC people are far more likely to live in neighborhoods that are under-resourced with inadequate housing, health facilities, schools, and financial opportunities. These neighborhoods are often food deserts and are impacted by industrial toxic exposures.
Mass incarceration. Disproportionately affecting people of color and the poor, U.S. hyper-incarceration harms the physical and mental health of millions of incarcerated people, tens of millions of their families, and injures countless communities (Young & Miller, 2020).
Structural impoverishment. Racism in the U.S. has resulted in at least three major factors that drive generational impoverishment of Black people and other people of color: Redlining and segregation to disenfranchised neighborhoods, denial of mortgage lending and exclusion from home ownership (the single most important factor in generational wealth), and hyper-incarceration that impoverishes individuals, families, and communities through the loss of income, job opportunities, and draconian financial penalties.
Racism is biologically toxic. Black and indigenous individuals have pregnancy-related mortality rates about three and two times higher, respectively, compared to the rate for White individuals (41.4 and 26.5 vs. 13.7 per 100,000 live births). Infants born to Black people are over twice as likely to die relative to those born to White people (10.4 vs. 4.4 per 1,000), and the mortality rate for infants born to American Indian and Alaska Native (AIAN) and Asian, Native Hawaiian, and Other Pacific Islander (NHOPI) people (7.7 and 7.2 per 1,000) is nearly twice as high (Hill & Artiga, 2022).
In addition to racism driving discrimination, poverty,
and exclusion from health resources, the lived experience of
this particular type of oppression is one of toxic stress and
generational trauma. Growing evidence supports the weathering
hypothesis, which states that chronic exposure to social and
economic disadvantage accelerates disease onset, disease
severity, aging, and death.
Healthcare access is a multidimensional concept that includes the availability of care, affordability, accommodation to the needs of patients and their communities ("after hours" and community-based care), the convenience of access with reasonable transportation requirements, and acceptability of care delivery that is culturally sensitive, trauma informed, and sensitive to historic injuries of a community.
BIPOC members of our communities are more likely to lack
health insurance (Artiga & Hill, 2020). Also, they are more
likely to live in neighborhoods without primary care and other
health services. Mistreatment by healthcare providers will
undermine trust and produce avoidance of health resources.
Even when BIPOC people have access to healthcare, government
statistics and healthcare research demonstrate that care is
inferior to that of Whites at every level of patient income.
For example, clinician communication is poorer, optimal
screenings and interventions are not offered, or pain is not
appropriately treated. Intersectionality of minoritized race
with every other social determinant of poor health worsens
health outcomes.
The meaning of health advocacy for clinicians. As stated by the World Health Organization, "health equity is achieved when everyone can attain their full potential for health and well-being." Maslow and other humanistic psychologists pointed to the multidimensionality of human needs that include physiological, social safety and security, love and belonging, self-esteem, self-expression and actualization of one’s human potential, and spiritual connection.
Being a health advocate means working to assure patient access
to the determinants of survival and total health. This includes
access to quality healthcare and also access to resources such
as nutritious food, safe housing, quality education, a living
wage, social connection, freedom from discrimination, and
equitable social opportunities.
Clinician health advocacy can happen at various levels:

At the level of direct patient interactions, this means actions that build trust and create social safety, screen for social needs and connect to resources, assure high-quality communication and best practices, and interrupt intentional or unconsciously biased behavior.
At the community and public policy levels of macro-advocacy, this means "promoting those social, economic, educational, and political changes that ameliorate the suffering and threats to human health and well-being that he or she identifies through his or her professional work and expertise" (AMA Declaration of Professional Responsibility, 2001).
Social determinants of health and survival are more powerful than healthcare in determining health outcomes.
Racism is a determinant of disease severity and premature death.
Multiple race-based factors prevent access to quality healthcare and social determinants of health and survival.
Intersectionality of race with other social risks is associated with even worse health inequities.
Health advocacy means promoting access to the determinants of health and survival at the patient, healthcare team, institution, community, and wider public policy levels.
Student advocacy in clinical education: Misrepresentation of race in clinical training is well documented. Consider the table below (Amutach, et al., 2021).
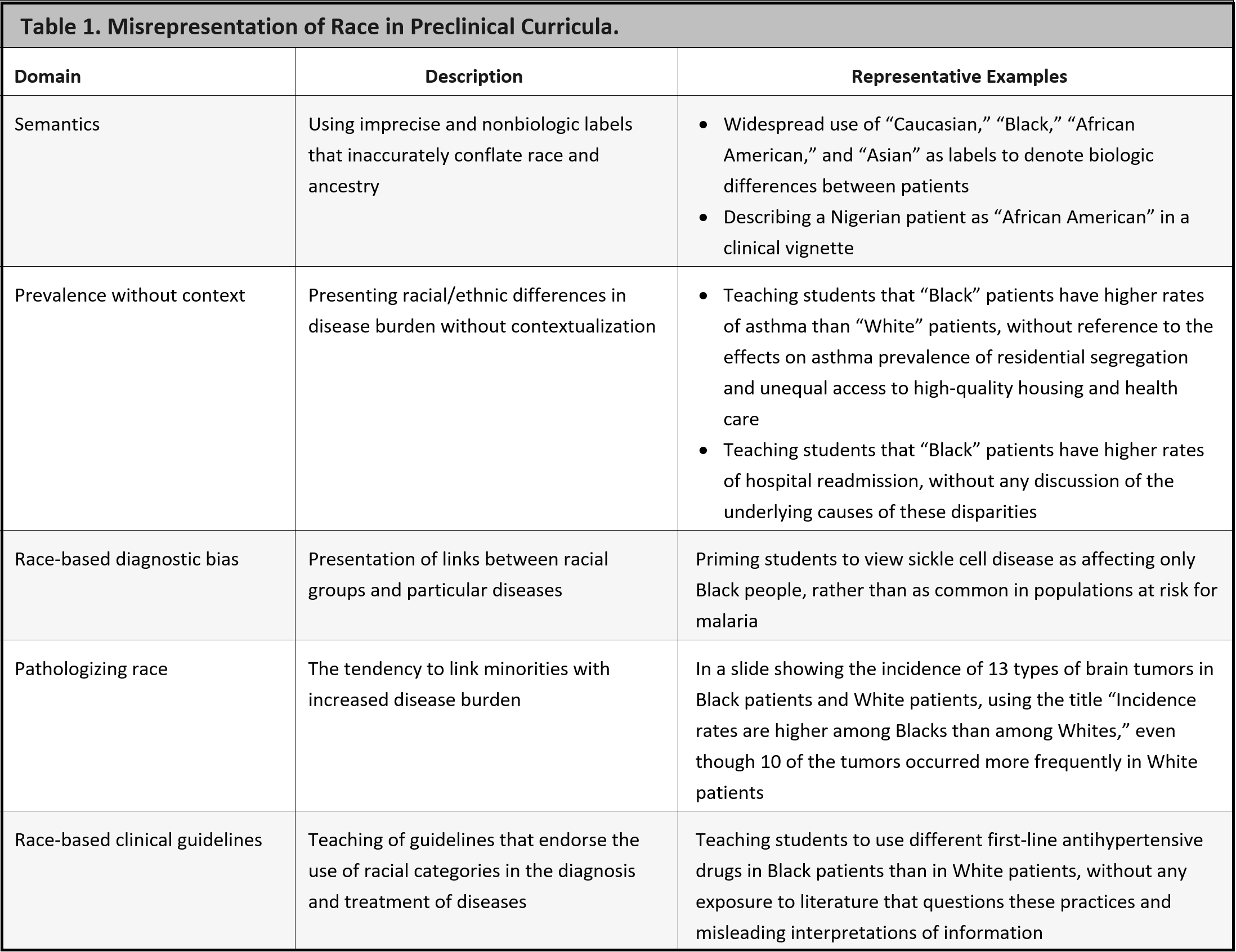
Source: https://www.nejm.org/doi/full/10.1056/nejmms2025768
Writing for advocacy is a valuable skill. Examples include:
- Writing a letter to a decision-maker in your institution.
- Tweeting and posting to get a message out.
- Writing a letter to the editor or op-ed to raise public awareness or influence public perception.
- Writing to a legislator.
While each of these may vary in style, there are very helpful, general guidelines. (The following are adapted from the National Consumer Voice for Quality Long-term Care):
- Lead in: Open with a statement that grabs attention right away.
- Present the problem, whom it affects, and its impact. Give an example or tell a little story that puts a face on the issue or makes it real.
- Provide three facts.
- "Some might say" – state the counterargument and refute it.
- Connect the issue to the audience's values, concerns, or self-interest.
- Make your request (the "ask") and be specific about what you want.
You can make a difference at all levels of advocacy through your commitment to diversity, equity, and inclusion in patient care. You can advocate for your individual patients, and you can have a wider impact as well. You can work with like-minded colleagues to change policy and procedures in your institution and the broader community. Remember Margaret Mead’s admonition: "Never doubt that a small group of thoughtful, committed citizens can change the world; indeed, it’s the only thing that ever has."
Centers for Disease Control and Prevention (CDC): https://www.cdc.gov/healthequity/features/maternal-mortality/index.html
- explain how structural, cultural, and individual racism have shaped our common history and have led to vast societal disparities in education, policing, wealth and healthcare;
- commit to being antiracist in your attitudes and behaviors;
- contribute to creating an antiracist learning culture for healthcare trainees that honors diversity, equity and inclusion: where all trainees are respected, where faculty model respect and empathy for all patients, colleagues and staff, and where trainees feel empowered to contribute to a culture of mutual learning;
- provide examples of how your increased self-awareness and reflection have helped you recognize your individual and cultural biases and how you use this awareness to seek to understand and empathize with your patients and clients of color, and to deliver equitable care to all;
- have the moral courage to act as an ally and upstander for your minoritized colleagues and patients;
- use your understanding of structural, cultural and individual biases to advocate for positive changes in your institutions and communities that will lead to equitable care for all.
So You Want to Talk About Race by Ijeoma Oluo (book).
Waking Up White by Debbie Iriving (book).
Raising White Kids by Jennifer Harvey (book).
The New Jim Crow: Mass Incarceration in the Age of Colorblindness by
Michelle Alexander (book).
How to Be An Antiracist by Ibram X Kendi (book)
Seeing White (Podcast)
Vital Voices (A podcast series from the Josiah Macy Foundation)
National Center for Health Statistics (US). Health, United States, 2015: With Special Feature on Racial and Ethnic Health Disparities. Hyattsville (MD): National Center for Health Statistics (US); 2016 May. Report No.: 2016-1232. PMID: 27308685. Phillips, K. W. (2014). How diversity makes us smarter. Scientific American, 311(4), 43-47.
Association, A. M. (2021). AMA’s Organizational Strategic Plan to
Embed Racial Justice and Advance Health Equity, 2021–2023. American
Medical Association. https://www.ama-assn.org/about/leadership/ama-s-strategic-plan-embed-racial-justice-and-advance-health-equity
Bellis, M. A., Hughes, K., Ford, K., Ramos Rodriguez, G., Sethi, D., & Passmore, J. (2019).
Life course health consequences and associated annual costs
of adverse childhood experiences across Europe and North America:
a systematic review and meta-analysis. Lancet Public Health, 4(10),
e517-e528. https://doi.org/10.1016/S2468-2667(19)30145-8
Byrd, W. M., & Clayton, L. A. (2001). Race, medicine, and health care in
the United States: a historical survey. J Natl Med Assoc, 93(3 Suppl),
11S-34S. https://www.ncbi.nlm.nih.gov/pubmed/12653395
Cooper, L. A., Roter, D. L., Carson, K. A., Beach, M. C.,
Sabin, J. A., Greenwald, A. G., & Inui, T. S. (2012). The
associations of clinicians' implicit attitudes about race
with medical visit communication and patient ratings of interpersonal
care. Am J Public Health, 102(5),
979-987. https://doi.org/10.2105/AJPH.2011.300558
Dyrbye, L., Herrin, J., West, C. P., Wittlin, N. M., Dovidio, J.
F., Hardeman, R., Burke, S. E., Phelan, S., Onyeador, I. N., Cunningham,
B., & van Ryn, M. (2019). Association of Racial Bias With Burnout Among
Resident Physicians. JAMA Netw Open, 2(7),
e197457. https://doi.org/10.1001/jamanetworkopen.2019.7457
Filut, A., Alvarez, M., & Carnes, M. (2020). Discrimination Toward Physicians
of Color: A Systematic Review. J Natl Med Assoc, 112(2),
117-140. https://doi.org/10.1016/j.jnma.2020.02.008
FitzGerald, C., & Hurst, S. (2017). Implicit bias in healthcare
professionals: a systematic review. BMC Med Ethics, 18(1),
19. https://doi.org/10.1186/s12910-017-0179-8
Hardeman, R. R., Perry, S. P., Phelan, S. M., Przedworski, J.
M., Burgess, D. J., & van Ryn, M. (2016). Racial Identity and
Mental Well-Being: The Experience of African American Medical
Students, A Report from the Medical Student CHANGE Study. J Racial
Ethn Health Disparities, 3(2),
250-258. https://doi.org/10.1007/s40615-015-0136-5
Hill, K. A., Samuels, E. A., Gross, C. P., Desai, M. M., Sitkin Zelin, N.,
Latimore, D., Huot, S. J., Cramer, L. D., Wong, A. H., & Boatright, D. (2020).
Assessment of the Prevalence of Medical Student Mistreatment by Sex,
Race/Ethnicity, and Sexual Orientation. JAMA Intern Med, 180(5),
653-665. https://doi.org/10.1001/jamainternmed.2020.0030
Hoffman, K. M., Trawalter, S., Axt, J. R., & Oliver, M. N. (2016).
Racial bias in pain assessment and treatment recommendations, and
false beliefs about biological differences between blacks and whites.
Proc Natl Acad Sci U S A, 113(16),
4296-4301. https://doi.org/10.1073/pnas.1516047113
Kendi, I. X. (2016). Stamped from the Beginning: The Definitive
History of Racist Ideas in America Bold Type Books.
Maina, I. W., Belton, T. D., Ginzberg, S., Singh, A., & Johnson, T. J.
(2018). A decade of studying implicit racial/ethnic bias in healthcare
providers using the implicit association test. Soc Sci Med, 199,
219-229. https://doi.org/10.1016/j.socscimed.2017.05.009
Tsai, J., Ucik, L., Baldwin, N., Hasslinger, C., & George, P. (2016). Race
Matters? Examining and Rethinking Race Portrayal in Preclinical Medical
Education. Acad Med, 91(7),
916-920. https://doi.org/10.1097/ACM.0000000000001232
Wheeler, R. M., Foster, J. W., & Hepburn, K. W. (2014). The experience of
discrimination by US and Internationally educated nurses in hospital practice
in the USA: a qualitative study. J Adv Nurs, 70(2),
350-359. https://doi.org/10.1111/jan.12197
Williams, D. R., Lawrence, J. A., & Davis, B. A. (2019). Racism and Health:
Evidence and Needed Research. Annu Rev Public Health, 40,
105-125. https://doi.org/10.1146/annurev-publhealth-040218-043750
Alang, S. M. (2019). Mental health care among blacks in America: Confronting
racism and constructing solutions. Health Serv Res, 54(2),
346-355. https://doi.org/10.1111/1475-6773.13115
Arias, E., Tejada-Vera, B., & Ahmad, F. (2021, February 2021).
Provisional Life Expectancy Estimates for January through June, 2020.
National Center for Health Statistics. Retrieved
4/2/22 from https://www.cdc.gov/nchs/data/vsrr/VSRR10-508.pdf
Eylem, O., de Wit, L., van Straten, A., Steubl, L., Melissourgaki, Z.,
Danisman, G. T., de Vries, R., Kerkhof, A., Bhui, K., & Cuijpers, P.
(2020). Stigma for common mental disorders in racial minorities and
majorities a systematic review and meta-analysis. BMC Public Health,
20(1), 879. https://doi.org/10.1186/s12889-020-08964-3
Lewis, T. T., Cogburn, C. D., & Williams, D. R. (2015). Self-reported experiences
of discrimination and health: scientific advances, ongoing controversies, and
emerging issues. Annu Rev Clin Psychol, 11,
407-440. https://doi.org/10.1146/annurev-clinpsy-032814-112728
Paradies, Y., Ben, J., Denson, N., Elias, A., Priest, N., Pieterse, A., Gupta, A.,
Kelaher, M., & Gee, G. (2015). Racism as a Determinant of Health: A Systematic
Review and Meta-Analysis. PLoS One, 10(9),
e0138511. https://doi.org/10.1371/journal.pone.0138511
Prevention, C. f. D. C. a. (2022, 3/25/22). Risk for COVID-19 Infection,
Hospitalization, and Death By Race/Ethnicity. CDC. Retrieved
4/2/22 from https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-race-ethnicity.html#print
Stringhini, S., Carmeli, C., Jokela, M., Avendano, M., Muennig, P., Guida, F.,
Ricceri, F., d'Errico, A., Barros, H., Bochud, M., Chadeau-Hyam, M., Clavel-Chapelon,
F., Costa, G., Delpierre, C., Fraga, S., Goldberg, M., Giles, G. G., Krogh, V.,
Kelly-Irving, M., . . . consortium, L. (2017). Socioeconomic status and the
25 x 25 risk factors as determinants of premature mortality: a
multicohort study and meta-analysis of 1.7 million men and women.
Lancet, 389(10075),
1229-1237. https://doi.org/10.1016/S0140-6736(16)32380-7
Thames, A. D., Irwin, M. R., Breen, E. C., & Cole, S. W. (2019). Experienced
discrimination and racial differences in leukocyte gene expression.
Psychoneuroendocrinology, 106,
277-283. https://doi.org/10.1016/j.psyneuen.2019.04.016
Williams, D. R., Lawrence, J. A., & Davis, B. A. (2019). Racism and Health:
Evidence and Needed Research. Annu Rev Public Health, 40,
105-125. https://doi.org/10.1146/annurev-publhealth-040218-043750
Williams, D. R., Lawrence, J. A., Davis, B. A., & Vu, C. (2019).
Understanding how discrimination can affect health. Health Serv Res,
54 Suppl 2, 1374-1388. https://doi.org/10.1111/1475-6773.13222
Yearby, R., Clark, B., & Figueroa, J. F. (2022). Structural Racism In
Historical And Modern US Health Care Policy. Health Aff (Millwood),
41(2), 187-194. https://doi.org/10.1377/hlthaff.2021.01466
American Psychiatric Association (2013). Diagnostic and Statistical Manual
of Mental Disorders, 5th Edn. Washington, DC: American Psychiatric Publishing.
Erikson, E. H. (1993). Childhood and society. New York: Norton; Chicago
Kahneman, Daniel. (2011) Thinking, Fast and Slow. New York:
Farrar, Straus and Giroux.
Kegan, Robert (1982) The evolving self: problem and process in human
development. Harvard University Press, Cambridge, MA
Ryan, R. M.; Deci, E. L. (2000). "Self-determination theory and the
facilitation of intrinsic motivation, social development, and well-being".
American Psychologist. 55 (1): 68–78
Vaillant, G. E. (1977). Adaptation to Life. Boston, MA: Little, Brown
Vaillant, G. E. (2008). Spiritual evolution: A scientific defense of faith. Broadway Book
Bowleg, L. (2012) The problem with the phrase women and minorities:
intersectionality-an important theoretical framework for public
health Am J Public Health, 102 1267-73
Tsai, J., Lindo, E., & Bridges, K. (2021). Seeing the Window, Finding the Spider:
Applying Critical Race Theory to Medical Education to Make Up Where Biomedical
Models and Social Determinants of Health Curricula Fall Short. Front Public
Health, 9, 653643. https://doi.org/10.3389/fpubh.2021.653643
Wesp, L. M., Scheer, V., Ruiz, A., Walker, K., Weitzel, J., Shaw, L., Kako, P.
M., & Mkandawire-Valhmu, L. (2018). An Emancipatory Approach to Cultural
Competency: The Application of Critical Race, Postcolonial, and
Intersectionality Theories. ANS Adv Nurs Sci, 41(4),
316-326. https://doi.org/10.1097/ANS.0000000000000230
Wikipedia. https://en.wikipedia.org/wiki/Colonialism
Vyas, D. A. , Eisenstein, L. G., Jones, D. S. (2020) Hidden in
Plain Sight - Reconsidering the Use of Race Correction in Clinical
Algorithms N Engl J Med 2020 Vol. 383 Issue 9 Pages 874-882. The full
article can be accessed
at: https://www.nejm.org/doi/full/10.1056/NEJMms2004740
Cruess, S. R., Johnston, S., & Cruess, R. L. (2004). "Profession": a
working definition for medical educators. Teaching and learning in
medicine, 16(1),
74–76. https://doi-org.proxy.library.vcu.edu/10.1207/s15328015tlm1601_15
Gameon, J. A., & Skewes, M. C. (2020). A Systematic Review of Trauma Interventions
in Native Communities. American journal of community psychology, 65(1-2),
223–241. https://doi.org/10.1002/ajcp.12396
Hoffman, K. M., Trawalter, S., Axt, J. R., & Oliver, M. N. (2016). Racial bias in
pain assessment and treatment recommendations, and false beliefs about biological
differences between blacks and whites. Proceedings of the National Academy of
Sciences of the United States of America, 113(16),
4296–4301. https://doi.org/10.1073/pnas.1516047113
Lazar, A. (2021). La operación: Coerced Sterilization of Puerto Rican
Women in the 20th Century and the Complexity of
Free Choice. https://digitalworks.union.edu/cgi/viewcontent.cgi?article=3530&context=theses
Accessed 5/7/2022
Miller, F. and Miller, P. (2021) Transgenerational trauma and trust restoration.
AMA Journal of Ethics. 23(6): E480-486. Doi:10.1001/amajethics.2021.480.
Patel, R. and Nagata, D. (2021) Historical trauma and descendants' wellbeing.
AMA Journal of Ethics. 23(6): E487-493. Doi: 10.1001/amajethics.2021.487
Perez-Rodriguez, J., & de la Fuente, A. (2017). Now is the Time for a Postracial
Medicine: Biomedical Research, the National Institutes of Health, and the Perpetuation
of Scientific Racism. The American journal of bioethics: AJOB, 17(9),
36–47. https://doi-org.proxy.library.vcu.edu/10.1080/15265161.2017.1353165
Powell, W., Richmond, J., Mohottige, D., Yen, I., Joslyn, A., & Corbie-Smith,
G. (2019). Medical mistrust, racism, and delays in preventive health screening
among African-American men. Behavioral Medicine, 45(2), 102-117.
Schmidt, H., Roberts, D. E., & Eneanya, N. D. (2022). Rationing, racism and justice:
advancing the debate around 'colourblind' COVID-19 ventilator allocation.
Journal of medical ethics, 48(2), 126–130.
https://doiorg.proxy.library.vcu.edu/10.1136/medethics-2020-106856
Schulman, K. A., Berlin, J. A., Harless, W. et al (1999) The effect of race and sex
on physicians' recommendations for cardiac catheterization. N Engl J Med 340,
618-26 https://www.nejm.org/doi/full/10.1056/nejm199902253400806
Smedley, B.D., Stith, A.Y., Nelson, A.R. (Eds) (2003) Unequal Treatment: Confronting
Racial and Ethnic Disparities in Health Care Institute of Medicine (US)
Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health
Care, Washington (DC): National Academies Press (US); 2003.PMID: 25032386,
Bookshelf ID: NBK220358, DOI: 10.17226/12875
Spector‐Bagdady, K., & Lombardo, P. A. (2019). US Public health service STD
experiments in Guatemala (1946–1948) and their aftermath. Ethics & Human Research,
41(2), 29-34. https://onlinelibrary.wiley.com/doi/10.1002/eahr.500010)
Warren, R. C., Shedlin, M. G., Alema-Mensah, E., Obasaju, C., & Hodge Sr, D. A.
(2019). Clinical trials participation among African Americans and the ethics of
trust: Leadership perspectives. Ethics, Medicine and Public Health, 10, 128-138.
Warren, R. C., Forrow, L., Hodge Sr, D. A., & Truog, R. D. (2020).
Trustworthiness before trust—Covid-19 vaccine trials and the Black community.
New England Journal of Medicine, 383(22), e121.
Williams, R. L., Vasquez, C. E., Getrich, C. M., Kano, M., Boursaw, B., Krabbenhoft,
C., & Sussman, A. L. (2018). Racial/Gender Biases in Student Clinical Decision-Making:
a Mixed-Method Study of Medical School Attributes Associated with Lower Incidence of
Biases. Journal of general internal medicine, 33(12),
2056–2064. https://doi-org.proxy.library.vcu.edu/10.1007/s11606-018-4543-2
Delgado, R., & Stefancic, J. (2017). Critical race theory. New York University Press.
DiAngelo, R. (2018). White fragility: Why it's so hard for white people to
talk about racism. Beacon Press. Hooks, b., Mesa-Bains, A. (2006) Homegrown: engaged cultural criticism. Cambridge, MA: South End Press
McIntosh, P. (1989) White Privilege: Unpacking the Invisible Knapsack,
Peace and Freedom
https://psychology.umbc.edu/files/2016/10/White-Privilege_McIntosh-1989.pdf
(accessed 5/7/22)
Morgan, K.P. (1996) Describing the Emperor's New Clothes: Three Myths of
Educational (In-)Equity ImprintRoutledge,
eBook ISBN9780429496530
Romano, M. J. (2018). White privilege in a white coat: how racism shaped my medical
education. The Annals of Family Medicine, 16(3), 261-263
Watts, R. J. (2003). Race consciousness and the health of African Americans.
Online Journal of Issues in Nursing, 8(1).
Hagiwara, N., Lafata, J. E., Mezuk, B., Vrana, S. R., & Fetters, M. D. (2019).
Detecting implicit racial bias in provider communication behaviors to reduce
disparities in healthcare: challenges, solutions, and future directions for
provider communication training. Patient education and counseling,
102(9), 1738-1743.
Hess, L., Palermo, A. G., & Muller, D. (2020). Addressing and undoing
racism and bias in the medical school learning and work environment.
Academic Medicine, 95(12S), S44-S50.
Johnson-Agbakwu, C. E., Ali, N. S., Oxford, C. M., Wingo, S., Manin, E., &
Coonrod, D. V. (2020). Racism, COVID-19, and Health Inequity in the USA: a
Call to Action. Journal of racial and ethnic health disparities, 1-7.
Ricks, T. N., Abbyad, C., & Polinard, E. (2021). Undoing racism and
mitigating bias among healthcare professionals: Lessons learned during a
systematic review. Journal of racial and ethnic health disparities, 1-11.
Sim, W., Lim, W. H., Ng, C. H., Chin, Y. H., Yaow, C. Y. L., Cheong, C. W.
Z., ... & Chong, C. S. (2021). The perspectives of health professionals and
patients on racism in healthcare: A qualitative systematic review.
PloS one, 16(8), e0255936.
Abrams, Z. (2022, January). Prominent issues in health care: Racial bias and
inequities. Monitor on Psychology,
53(1). https://www.apa.org/monitor/2022/01/special-prominent-issues
Burke, S. E., Dovidio, J. F., Perry, S. P., Burgess, D. J., Hardeman, R. R.,
Phelan, S. M., Cunningham, B. A., Yeazel, M. W., Przedworski, J. M., & van
Ryn, M. (2017). Informal Training Experiences and Explicit Bias against
African Americans among Medical Students. Social Psychology Quarterly, 80(1),
65–84. https://doi.org/10.1177/0190272516668166
Goleman, Daniel (1996). Emotional Intelligence: Why It Can Matter More Than IQ.
Bantam Books.
Griffith, D.M., Mason, M., Yonas, M. et al. Dismantling institutional
racism: theory and action. Am J Community Psychol 39,
381–392 (2007). https://doi.org/10.1007/s10464-007-9117-0
Nixon, S.A. The coin model of privilege and critical allyship: implications
for health. BMC Public Health 19, 1637
(2019). https://doi.org/10.1186/s12889-019-7884-9
Penner LA, Blair IV, Albrecht TL, Dovidio JF. Reducing Racial Health Care
Disparities: A Social Psychological Analysis. Policy insights from the
behavioral and brain sciences. 2014;1(1):204-212.
doi:10.1177/2372732214548430
Sue, D. W. (2010). Microaggressions in everyday life: Race, gender, and
sexual orientation. John Wiley & Sons.
The Science of Equality Volume 1: Addressing Implicit Bias, Racial Anxiety,
and Stereotype Threat in Education and Health Care. (2014). In Medical
Benefits (Vol. 31, Issue 23, p. 12–). Aspen Publishers, Inc.
Cheung, F., Ganote, C. M., & Souza, T.J. (2016). Microaggressions and
microresistance: Supporting and empowering students. Faculty Focus Special
Report: Diversity and Inclusion in the College Classroom. Magna
Publication. http://ww1.facultyfocus.com/register/free-reports/main.html?product_id=520 .
Freeman, L., & Stewart, H. (2018). Microaggressions in clinical medicine.
Kennedy Institute of Ethics Journal, 28(4), 411-449.
Overland, M. K., Zumsteg, J. M., Lindo, E. G., Sholas, M. G., Montenegro,
R. E., Campelia, G. D., & Mukherjee, D. (2019). Microaggressions in clinical
training and practice. Pm&r, 11(9), 1004-1012.
Sue, D. W. (2010). Microaggressions in everyday life: Race, gender,
and sexual orientation. John Wiley & Sons.
Sue, D. W., Alsaidi, S., Awad, M. N., Glaeser, E., Calle, C. Z., &
Mendez, N. (2019). Disarming racial microaggressions: Microintervention
strategies for targets, White allies, and bystanders. American
Psychologist, 74(1), 128.
Discrimination. Amnesty International. (2021, June 1).
Retrieved from https://www.amnesty.org/en/what-we-do/discrimination/
History.com Staff. (2018, August 24). Chinese Exclusion Act.
History.com. Retrieved from https://www.history.com/topics/immigration/chinese-exclusion-act-1882
Indian Removal Act, S. 102, 21st Cong. (1930). A Century of Lawmaking for a
New Nation: U.S. Congressional Documents and Debates, 1774 - 1875 (21AD).
The Library of Congress. Retrieved
from https://memory.loc.gov/cgi-bin/ampage?collId=llsl&fileName=004/llsl004.db&recNum=458 .
Lang, K., & Kahn-Lang Spitzer, A. (2020). Race Discrimination: An Economic
Perspective. Journal of Economic Perspectives, 34(2), 68–89.
Lewsley, J., & White, M. (2020, July 28). The effects of racism on health
and mental health. Medical News Today.
Retrieved from https://www.medicalnewstoday.com/articles/effects-of-racism#adults
MacIntosh T, Desai MM, Lewis TT, Jones BA, Nunez-Smith M (2013). Socially-Assigned
Race, Healthcare Discrimination and Preventive Healthcare Services.
PLoS ONE 8(5): e64522. doi:10.1371/journal.pone.0064522
Mejia, M. (2021, July 18). The U.S. history of Native American Boarding
Schools. The Indigenous Foundation. Retrieved
from https://www.theindigenousfoundation.org/articles/us-residential-schools
Nieblas-Bedolla, Edwin MPH; Christophers, Briana; Nkinsi, Naomi T.;
Schumann, Paul D.; Stein, Elizabeth (2020). Changing How Race Is Portrayed
in Medical Education: Recommendations From Medical Students, Academic Medicine:
December 2020 - Volume 95 - Issue 12 - p 1802-1806 doi: 10.1097/ACM.0000000000003496
Pascoe, E., & Richman, L. (2009). Perceived Discrimination and Health: A
Meta-Analytic Review. Psychological Bulletin, 135(4), 531–554.
Roediger, D. (2021, December 16). Historical Foundations of Race. National
Museum of African American History and Culture. Retrieved
from https://nmaahc.si.edu/learn/talking-about-race/topics/historical-foundations-race
Sabin, J. A., Nosek, B. A., Greenwald, A. G., & Rivara, F. P. (2009).
Physicians’ implicit and explicit attitudes about race by MD race, ethnicity,
and gender. Journal of Healthcare for the Poor and Underserved, 20, 896-913.
Shah, K., & Adolphe, J. (2019, August 16). 400 years since slavery:
A timeline of American history. The Guardian. Retrieved
from https://www.theguardian.com/news/2019/aug/15/400-years-since-slavery-timeline
Small, M., & Pager, D. (2020). Sociological Perspectives on Racial
Discrimination. Journal of Economic Perspectives, 34(2), 49–67.
Smedley BD, Stith AY, Nelson AR, editors (2003) Unequal Treatment:
Confronting Racial and Ethnic Disparities in Health Care. Washington, DC:
National Academies Press.764 p.
Chou C., Pearlman E., Risdon. 2014 Understanding Difference and
Diversity in the Medical Encounter: Communication Across Cultures.
DocCom Module 15 https://webcampus.med.drexel.edu/DocCom/
Deliz, J. R., Fears, F. F., Jones, K. E., Tobat, J., Char, D., & Ross, W. R.
(2020). Cultural competency interventions during medical school: a scoping
review and narrative synthesis. Journal of general internal medicine, 35(2), 568-577.
Foronda, C. (2020). A theory of cultural humility.
Journal of Transcultural Nursing, 31(1), 7-12.
Josiah Macy Jr. Foundation. (2018). Improving environments for learning in
the health professions. Retrieved
from https://macyfoundation.org/assets/reports/publications/macy_mono-graph_2018_webfile.pdf
Leininger, M. M. (1988). Leininger’s theory of nursing: Cultural care
diversity and universality. Nursing Science Quarterly, 1, 152-160.
Tervalon, M., & Murray-García, J. (1998). Cultural humility versus
cultural competence: A critical distinction in defining physician
training outcomes in multicultural education. Journal of Health Care
for the Poor and Underserved, 9, 117-125. doi:10.1353/hpu.2010.0233
Yeager, K. A., & Bauer-Wu, S. (2013). Cultural humility: Essential
foundation for clinical researchers. Applied Nursing Research,
26, 251-256. doi:10.1016/j.apnr.2013.06.008
Healthy People 2030, U.S. Department of Health and Human Services,
Office of Disease Prevention and Health
Promotion. https://health.gov/healthypeople/objectives-and-data/social-determinants-health
Johnson, G. (2020). COVID-19’s assault on Black and Brown
communities. Penn Today.
National Academies of Sciences, Engineering, and Medicine; Health
and Medicine Division; Board on Population Health and Public Health
Practice; Committee on Community-Based Solutions to Promote Health
Equity in the United States; Baciu A, Negussie Y, Geller A, et al.,
editors. Communities in Action: Pathways to Health Equity. Washington
(DC): National Academies Press (US); 2017 Jan 11. 3, The Root Causes
of Health Inequity.
Available from: https://www.ncbi.nlm.nih.gov/books/NBK425845/
Paradies, Y., Ben, J., Denson, N., Elias, A., Priest, N., Pieterse,
A., ... & Gee, G. (2015). Racism as a determinant of health: a
systematic review and meta-analysis. PloS one, 10(9), e0138511.
Robert Wood Johnson
Foundation. https://www.rwjf.org/en/library/research/2017/05/what-is-health-equity-.html
Tiwari, T., Palatta, A., Stewart, J., Guidelines, P. M., &
Evidence Standards Working Group. (2020). What is the Value of Social
Determinants of Health in Dental Education?. NAM perspectives, 2020.
WHO. https://www.who.int/about/governance/constitution
Child trends.
https://www.childtrends.org/wp-content/uploads/2019/09/RacialEthnicEquityPerspective_ChildTrends_October2019.pdf
Child trends.
https://www.childtrends.org/publications/five-guiding-principles-for-integrating-racial-and-ethnic-equity-in-researchhttps://www.childtrends.org/publications/five-guiding-principles-for-integrating-racial-and-ethnic-equity-in-research
Hardeman, R., Medina, E., & Kozhimannil, K. B. (2016).
Dismantling structural racism, supporting Black lives, and achieving
health equity: The role of health professionals. New England Journal
of Medicine, 375(22), 2113–2115.
Heeju Sohn (2017). Racial and Ethnic Disparities in Health
Insurance Coverage: Dynamics of Gaining and Losing Coverage over
the Life-Course. Population Research Policy Review. 36(2): 181–201
Konkel L. (2015). Racial and Ethnic Disparities in Research Studies:
The Challenge of Creating More Diverse Cohorts. Environmental health
perspectives, 123(12), A297–A302. https://doi.org/10.1289/ehp.123-A297
Metzl, J. M., & Hansen, H. (2014). Structural competency: Theorizing a
new medical engagement with stigma and inequality. Social Science and
Medicine, 103, 126–133. https://doi.org/10.1016/j.socscimed.2013.06.032
Neff, J., Holmes, S. M., Knight, K. R., Strong, S., Thompson-Lastad, A.,
McGuinness, C., ... & Nelson, N. (2020). Structural competency: curriculum
for medical students, residents, and interprofessional teams on the structural
factors that produce health disparities. MedEdPORTAL, 16, 10888. Structural
competency: Curriculum for medical students, residents, and interprofessional
teams on the structural factors that produce health disparities.
Vyas, D. A. , Eisenstein, L. G., Jones, D. S. (2020) Hidden in Plain Sight -
Reconsidering the Use of Race Correction in Clinical Algorithms N Engl J
Med 2020 Vol. 383 Issue 9 Pages 874-882. The full article can be
accessed at: https://www.nejm.org/doi/full/10.1056/NEJMms2004740
Abby Ellin (2021). 'Death Doulas' Provide Aid at the End of Life
(Links to an external site.). The New York Times.
Ada Stewart (2019). Cultural Humility Is Critical to Health
Equity (Links to an external site.). American Academy of Family Physicians.
Amutah, C., Greenidge, K., Mante, A., Munyikwa, M., Surya, S. L.,
Higginbotham, E., ... & Aysola, J. (2021). Misrepresenting race—the
role of medical schools in propagating physician bias. New England
Journal of Medicine, 384(9), 872-878.Vyas D, Eisenstein L, Jones D,
Hidden in Plain Sight – Reconsidering the Use of Race Correction in
Clinical Algorithms, NEJM, 2020, DOI: 10.1056/NEJMms2004740
Cahn, P. S. (2020). How interprofessional collaborative practice
can help dismantle systemic racism. Journal of Interprofessional
Care, 34(4), 431-434.
Garran, A. M., & Rasmussen, B. M. (2019). How should organizations
respond to racism against health care workers?. AMA Journal of
Ethics, 21(6), 499-504.
Interprofessional Education Collaborative. (2016). Core competencies
for interprofessional collaborative practice: 2016 update. Washington, DC:
Interprofessional Education Collaborative.
Legha, R. K., & Miranda, J. (2020). An anti-racist approach to
achieving mental health equity in clinical care. Psychiatric Clinics, 43(3), 451-469.
Paul-Emile, K. (2019). How should organizations support
trainees in the face of patient bias?. AMA journal of ethics, 21(6), 513-520.
Paul-Emile, K., Smith, A. K., Lo, B., & Fernández, A. (2016).
Dealing with racist patients. New England J. Med., 374, 708.
Kendi, Ibram X. How to Be an Antiracist. New York, NY: One World, 2019.
Roberts, D. (2011). Fatal invention: How science, politics, and big
business re-create race in the twenty-first century. New Press/ORIM.
Tervalon, M., & Murray-Garcia, J. (1998). Cultural humility versus
cultural competence: A critical distinction in defining physician
training outcomes in multicultural education. Journal of health care
for the poor and underserved, 9(2), 117-125.
Tressie McMillan Cottom (2019). "I Was Pregnant and in Crisis.
All the Doctors and Nurses Saw Was an Incompetent Black Woman."
(Links to an external site.) Time.
World Professional Association for Transgender Health (WPATH)
(2012). Standards of Care, Version 7 (Links to an external site.).
Anne Bishop, Becoming an Ally, 3rd Edition: Breaking the Cycle of
Oppression in People. Fernwood Publishing, Halifax, 2015
Atcheson, S. (2018). Allyship-The Key To Unlocking The Power Of
Diversity. Forbes Magazine.
Burack, J.H., Irby, D.M., Carline, J.D., Root,R.K., and Larson, E. B. (1999)
Teaching Compassion and Respect: Attending Physicians’ Responses to Problematic
Behaviors. J Gen Intern Med. 14(1): 49–55.
Brown, K. T., & Ostrove, J. M. (2013). What does it mean to be an ally?:
The perception of allies from the perspective of people of color. Journal of
Applied Social Psychology, 43(11), 2211-2222.
Cihangir, S., Barreto, M., & Ellemers, N. (2014). Men as allies against sexism:
The positive effects of a suggestion of sexism by male (vs. female) sources. Sage
Open, 4(2), 2158244014539168.
Medium.com; Holiday Phillips May 9, 2020
Sue, D.W., Alsaidi, S., Awad, M.N., Glaeser, E., Calle, C.Z.,
Mendez, N. (2019) Disarming Racial Microaggressions: Microintervention
Strategies for Targets, White Allies, and Bystanders
American Psychologist 74, 128–142
Professor of Medicine
Associate Dean of Medical Education
Drexel University College of Medicine
Camille Burnett, PhD, MPA, APHN-BC, BScN, RN, DSW, FAAN, CGNC
Associate Vice President, Education and Health Equity
Executive Associate Director, Institute for Inclusion, Inquiry and Innovation
Office of Institutional Equity, Effectiveness and Success
Virginia Commonwealth University
Student
Virginia Commonwealth University School of Pharmacy
Janice H. Altman, PhD
Executive Director of IExcel Education
Office of Institutional Equity, Effectiveness and Success
Virginia Commonwealth University
Camille Burnett, PhD, MPA, APHN-BC, BScN, RN, DSW, FAAN, CGNC
Associate Vice President, Education and Health Equity
Executive Associate Director, Institute for Inclusion, Inquiry and Innovation
Office of Institutional Equity, Effectiveness and Success
Virginia Commonwealth University
Beverley A. Crawford, DDS
Director of Diversity and Inclusion
Associate Professor of Clinical Dentistry
Department of Preventive and Restorative Sciences
Penn Dental Medicine
University of Pennsylvania
Alice Fornari, EdD, FAMEE, RDN, HEC-C
Vice President Faculty Development
Northwell Health
Office of Academic Affairs
Associate Dean
Donald and Barbara Zucker School of Medicine At Hofstra Northwell
Janice Thomas John, DO, MS, MPH
Assistant Dean for Integrated Medical Education
Assistant Professor of Pediatrics
Albert Einstein College of Medicine
Dennis H. Novack, MD
Professor of Medicine
Associate Dean of Medical Education
Drexel University College of Medicine
Archana A. Pathak, PhD
Special Assistant, Programs & Initiatives
Interim Director, Q Collective
Office of Institutional Equity, Effectiveness and Success
Associate Professor
Dept. of Gender, Sexuality & Women's Studies
Virginia Commonwealth University
R. Ellen Pearlman, MD, FACH
Associate Dean for Professionalism & Doctoring Skills
Donald and Barbara Zucker School of Medicine at Hofstra/Northwell
Steven Rosenzweig, MD
Director, Office of Community Experience / Educational Affairs
Professor, Emergency Medicine (Hospice and Palliative Medicine)
Drexel University College of Medicine
Brooke Salzman, MD
Associate Provost of Interprofessional Practice and Education
Co-Director, Jefferson Center for Interprofessional Practice and Education
Professor
Department of Family and Community Medicine
Division of Geriatric Medicine and Palliative Care
Thomas Jefferson University
Lisa Webb, EdD, CRC
Assistant Vice President, Faculty Development, Recruitment and Retention
Office of the Senior Vice President for Health Sciences
Health Sciences Faculty Development Specialist, CTLE
Affiliate Faculty, School of Education
Virginia Commonwealth University
Becks Wilson
Academic Coordinator
Women's Health Education Program
Drexel University College of Medicine
Director - Diversity, Equity and Inclusion
Director of Ethics Curriculum & the Mirmelstein Lecture Associate Professor
Department of Dental Public Health and Policy
VCU School of Dentistry and VCU Dental Care
Rita Guevara, MD, FAAP
Assistant Dean of Diversity, Equity, and Inclusion, Drexel University College of Medicine
Director of Health Equity, St. Christopher’s Hospital for Children
Attending Physician, Section of General Pediatrics, St. Christopher’s Hospital for Children
Assistant Professor of Pediatrics, Drexel University College of Medicine
Kristen Ryczak, MD
Assistant Professor of Family Medicine
Director, Women's Health Education Program
Drexel University College of Medicine
Professor of Medicine
Associate Dean of Medical Education
Drexel University College of Medicine
Rita Guevara, MD FAAP
Assistant Dean of Diversity, Equity, and Inclusion, Drexel University College of Medicine
Director of Health Equity, St. Christopher’s Hospital for Children
Attending Physician, Section of General Pediatrics, St. Christopher’s Hospital for Children
Assistant Professor of Pediatrics, Drexel University College of Medicine
Leon McCrea II, MD, MPH, FAAFP
Associate Professor, Department of Family, Community, and Preventive Medicine
Senior Associate Dean of Diversity, Equity and Inclusion
Interim Program Director, Tower Health/Drexel University College of Medicine Family Medicine Residency
Director, Drexel Pathway to Medical School
Drexel University College of Medicine
MD/PhD Candidate | Class of 2026
Drexel University College of Medicine
Leila Hilal, MD
Drexel University College of Medicine graduate 2022
Gina Li
Drexel University College of Medicine
MD Candidate | Class of 2025
Kate J Morse, PhD, MSN, RN, CHSE, ACNP-Ret
Assistant Dean, Experiential Learning and Innovation
Associate Clinical Professor of Nursing
Drexel University College of Nursing & Health Professions
Alena Nixon
Drexel University College of Medicine
MD Candidate | Class of 2023
Kathy Phan, BSN, RN
Erica Riddick
MD Candidate | Class of 2024
Gene Dalessandro
Robyn Maloney-George
Donald Santman
Director of TIME
Technology in Medical Education
Bruce D. Wartman
Manager of Educational Development and Instructional Design
Technology in Medical Education
David Ross
Senior Multimedia Technician, Educational Resources
Breanna Ruiz
Audiovisual Technician
